- Joined
- Apr 6, 2013
- Messages
- 847
- Reaction score
- 415
67 yo guy
Totally normal, reasonable, very high functioning professional.
Has been having left arm radicular pain for several months. Noticing some weakness in the last month or two. Hard to carry books, drooped a few things etc. On exam some subtle weakness of grip strength/hand on that side, but still like 4.5/5.
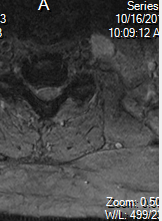
MRI below. I measured the AP canal diameter at that tightest level at around 9mm.
Has not done cervical traction/gabapentin or CESI.
Surgeon has him on for mid Decemeber for what sounds like a fusion. Said no point doing other stuff as surgery is going to have to happen.
What do you guys think? He is asking me if I would just have the surgery or try and hold off.
Seems like a tweener...

FINDINGS:
There is normal alignment without evidence of acute fracture or dislocation. Vertebral body heights are well maintained. Visualized cord is within normal limits. Normal marrow signal. Prevertebral soft tissues are unremarkable.
Individual disc levels are as follows:
C2-C3: Small posterior disc osteophyte complex and bilateral facet arthropathy resulting in mild spinal canal narrowing. There is mild bilateral neural foraminal narrowing.
C3-C4: Small posterior disc osteophyte complex with right lateral recess component and mild facet arthropathy resulting in mild to moderate spinal canal narrowing. There is moderate bilateral neural foraminal narrowing.
C4-C5: Small to moderate posterior disc osteophyte complex with right paracentral and lateral recess component resulting in moderate spinal canal narrowing and deformation of the ventral cord. There is moderate to severe right and mild left neural
foraminal narrowing.
C5-C6: Moderate posterior disc osteophyte complex and bilateral facet arthropathy resulting in severe spinal canal narrowing. There is severe right and moderate to severe left neural foraminal narrowing.
C6-C7: Moderate posterior disc osteophyte complex and bilateral facet arthropathy resulting in moderate to severe spinal canal narrowing. There is moderate to severe right and moderate left neural foraminal narrowing.
C7-T1: Mild disc desiccation without significant spinal canal or neural foraminal narrowing.
IMPRESSION:
Multilevel degenerative changes of the cervical spine as described, most pronounced at C5-C6 with severe spinal canal stenosis.
Neural foraminal stenosis as described.
Totally normal, reasonable, very high functioning professional.
Has been having left arm radicular pain for several months. Noticing some weakness in the last month or two. Hard to carry books, drooped a few things etc. On exam some subtle weakness of grip strength/hand on that side, but still like 4.5/5.
MRI below. I measured the AP canal diameter at that tightest level at around 9mm.
Has not done cervical traction/gabapentin or CESI.
Surgeon has him on for mid Decemeber for what sounds like a fusion. Said no point doing other stuff as surgery is going to have to happen.
What do you guys think? He is asking me if I would just have the surgery or try and hold off.
Seems like a tweener...
FINDINGS:
There is normal alignment without evidence of acute fracture or dislocation. Vertebral body heights are well maintained. Visualized cord is within normal limits. Normal marrow signal. Prevertebral soft tissues are unremarkable.
Individual disc levels are as follows:
C2-C3: Small posterior disc osteophyte complex and bilateral facet arthropathy resulting in mild spinal canal narrowing. There is mild bilateral neural foraminal narrowing.
C3-C4: Small posterior disc osteophyte complex with right lateral recess component and mild facet arthropathy resulting in mild to moderate spinal canal narrowing. There is moderate bilateral neural foraminal narrowing.
C4-C5: Small to moderate posterior disc osteophyte complex with right paracentral and lateral recess component resulting in moderate spinal canal narrowing and deformation of the ventral cord. There is moderate to severe right and mild left neural
foraminal narrowing.
C5-C6: Moderate posterior disc osteophyte complex and bilateral facet arthropathy resulting in severe spinal canal narrowing. There is severe right and moderate to severe left neural foraminal narrowing.
C6-C7: Moderate posterior disc osteophyte complex and bilateral facet arthropathy resulting in moderate to severe spinal canal narrowing. There is moderate to severe right and moderate left neural foraminal narrowing.
C7-T1: Mild disc desiccation without significant spinal canal or neural foraminal narrowing.
IMPRESSION:
Multilevel degenerative changes of the cervical spine as described, most pronounced at C5-C6 with severe spinal canal stenosis.
Neural foraminal stenosis as described.
Last edited:


