D
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
- Joined
- Apr 28, 2005
- Messages
- 1,198
- Reaction score
- 3,443
Article won’t load but fits with the radiation as the treatment of last resort mantra I’ve been seeing.
- Joined
- Sep 20, 2004
- Messages
- 11,743
- Reaction score
- 11,838
Really depends on the aggressiveness of your local CT surgeon and how comfortable pulmonary feels about SBRT etc. Make inroads with your pulmonologist colleagues. With CT lung screening, definitely have seen my lung SBRT caseload go up the last few yearsArticle won’t load but fits with the radiation as the treatment of last resort mantra I’ve been seeing.
- Joined
- Oct 24, 2010
- Messages
- 3,512
- Reaction score
- 6,365
Enjoy it now while you can…Really depends on the aggressiveness of your local CT surgeon and how comfortable pulmonary feels about SBRT etc. Make inroads with your pulmonologist colleagues. With CT lung screening, definitely have seen my lung SBRT caseload go up the last few years
Society of Interventional Radiology - Lung ablation position statement
The Society of Interventional Radiology issued a new position statement on percutaneous lung ablation with an accompanying quality improvement document that establishes performance thresholds for patient safety.
Get your biopsy and nodule treated all at once!
Surgeons should be grateful for SBRT. The Will Rogers phenomenon will only help their outcomes. Everyone wins! 😁
- Joined
- Jul 26, 2007
- Messages
- 12,692
- Reaction score
- 2,311
Really depends on the aggressiveness of your local CT surgeon and how comfortable pulmonary feels about SBRT etc. Make inroads with your pulmonologist colleagues. With CT lung screening, definitely have seen my lung SBRT caseload go up the last few years
At my new place the environment seems to favor surgery much more than my last.
Which is unfortunate because the surgeons are old, the patients are unhealthy and all smoke. I've been there two months and have already seen multiple local recurrences in 70+ year olds <1 year after surgery, all of which had worse lung function and chronic pain after surgery. Going to have to become the pulmonary best friend because if I can see them up front, they will choose SBRT.
- Joined
- Apr 3, 2019
- Messages
- 4,269
- Reaction score
- 9,961
This is the kind of data SBRT-hating insurance companies love.
- Joined
- Sep 20, 2004
- Messages
- 11,743
- Reaction score
- 11,838
Data is terrible on rfa and i suspect will continue to be so. Why get an ablation when you are skipping a biopsy with some frequency after shared decision making between you, patient and referring?Enjoy it now while you can…
Society of Interventional Radiology - Lung ablation position statement
The Society of Interventional Radiology issued a new position statement on percutaneous lung ablation with an accompanying quality improvement document that establishes performance thresholds for patient safety.www.sirweb.org
Get your biopsy and nodule treated all at once!
- Joined
- Jun 1, 2011
- Messages
- 628
- Reaction score
- 869
This article appears to be an ncdb analysis. Nothing to see here. VALOR will hopefully answer the question once and for all.
- Joined
- Oct 24, 2010
- Messages
- 3,512
- Reaction score
- 6,365
Haven’t we learned it’s never been about data. It’s always been about access and who is first in line in the pipeline. Now a days, patients are getting bombarded with advertisements and “data” from sources outside of medical journals. The data on protons isn’t great but the majority of my patients want it before they even see me.Data is terrible on rfa and i suspect will continue to be so. Why get an ablation when you are skipping a biopsy with some frequency after shared decision making between you, patient and referring?
The field of medicine has become a business in the worst way.

Advantages of Focal Laser Ablation To Treat Prostate Cancer
Learn about Focal Laser treatment for prostate cancer at the Sperling Prostate Center using the most powerful laser available.
I’m beginning to believe that our niche may just be in salvage settings since radiation is so “bad.”
Last edited:
- Joined
- Sep 20, 2004
- Messages
- 11,743
- Reaction score
- 11,838
I'm treating a decent number now where patients can't get or refuse a biopsy. The risks are the same if ablation is being consideredHaven’t we learned it’s never been about data. It’s always been about access and who is first in line in the pipeline. Now a days, patients are getting bombarded with advertisements and “data” from sources outside of medical journals. The data on protons isn’t great but the majority of my patients want it before they even see me.
The field of medicine has become a business in the worst way.

Advantages of Focal Laser Ablation To Treat Prostate Cancer
Learn about Focal Laser treatment for prostate cancer at the Sperling Prostate Center using the most powerful laser available.sperlingprostatecenter.com
I’m beginning to believe that our niche may just be in salvage settings since radiation is so “bad.”
- Joined
- Oct 24, 2010
- Messages
- 3,512
- Reaction score
- 6,365
I’m not debating if ablation is a better or a safer option, I’m just saying that there are more options available to patients and not every provider will think about the best clinical outcome for patients.
My argument is that there will be a time where we are not even considered an option in most early stage cancers. You may have a good situation but I believe that the future isn’t looking good in our field unless we find ways to adapt and not believe that having good “data” will save our field.
While all these things are going on, rad oncs will figure out ways to make radiation less utilized unless it’s to go on some expensive machine or figuring out ways to make everything into one fraction or less.
My argument is that there will be a time where we are not even considered an option in most early stage cancers. You may have a good situation but I believe that the future isn’t looking good in our field unless we find ways to adapt and not believe that having good “data” will save our field.
While all these things are going on, rad oncs will figure out ways to make radiation less utilized unless it’s to go on some expensive machine or figuring out ways to make everything into one fraction or less.
Last edited:
If the SBRT + immunotherapy trials show improved outcomes, then there’s no way IR ablation for early stage NSCLC will take off. Not just from an evidence perspective—then med oncs will have skin in the game too.I’m not debating if ablation is a better or a safer option, I’m just saying that there are more options available to patients and not every provider will think about the best clinical outcome for patients.
My argument is that there will be a time where we are not even considered an option in most early stage cancers. You may have a good situation but I believe that the future isn’t looking good in our field unless we find ways to adapt and not believe that having good “data” will save our field.
While all these things are going on, rad oncs will figure out ways to make radiation less utilized unless it’s to go on some expensive machine or figuring out ways to make everything into one fraction or less.
- Joined
- Jul 14, 2020
- Messages
- 1,374
- Reaction score
- 4,158
Not meaningful at all. Selection bias can even work in this environment. The standards for medical resectability are broad. Most centers will still recommend surgery for apparently fit patients (I do) and those that go against recommendations are subject to all of the ills that befall contrarians.This article appears to be an ncdb analysis. Nothing to see here. VALOR will hopefully answer the question once and for all.
A little like the early second malignancy data for proton prostate patients. Your smokers by and large ain’t getting protons.
If you refuse a recommended surgery, are you going to get your AAA repaired?
Last edited:
- Joined
- Oct 24, 2010
- Messages
- 3,512
- Reaction score
- 6,365
I’m hoping you’re right but I don’t see our field gaining new ground in any disease site except for palliation/salvage and oligomets.If the SBRT + immunotherapy trials show improved outcomes, then there’s no way IR ablation for early stage NSCLC will take off. Not just from an evidence perspective—then med oncs will have skin in the game too.
All of the definitive treatments, I can see being mismanaged first by all the specialists who see the patient before we do.
This article appears to be an ncdb analysis. Nothing to see here. VALOR will hopefully answer the question once and for all.
There are multiple meta analysis floating around. It’s impossible to control for the biases inherent in those types of studies. Most either show equivalence or surgery better. I’m excluding stars rosel because it’s small.
It’s the same with surg vs RT for prostate cancer. Plenty of surgically driven meta analysis saying surgery is better not surprisingly.
- Joined
- Sep 20, 2004
- Messages
- 11,743
- Reaction score
- 11,838
Biggest issue with ablation is the same reason why biopsies have transitioned from transthoracic CT-guided biopsy to enb biopsies. Pneumothorax rate of 25-50% is no joke and if patients think they weren't given an option for sbrt after they end up in the hospital with a chest tube overnight, well it's going to get out eventuallyI’m not debating if ablation is a better or a safer option, I’m just saying that there are more options available to patients and not every provider will think about the best clinical outcome for patients.
My argument is that there will be a time where we are not even considered an option in most early stage cancers. You may have a good situation but I believe that the future isn’t looking good in our field unless we find ways to adapt and not believe that having good “data” will save our field.
While all these things are going on, rad oncs will figure out ways to make radiation less utilized unless it’s to go on some expensive machine or figuring out ways to make everything into one fraction or less.
I've heard of endobronchial ablation as a possibility given increasing electronavigational bronchoscopies but that seems to be more palliative than definitive from what i can tell. Pulmonologists around here aren't sending out for transthoracic biopsies as much here, so not sure why they would all of a sudden start doing more transthoracic ablations 🤷♂️
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
This article appears to be an ncdb analysis. Nothing to see here. VALOR will hopefully answer the question once and for all.
i hate to be debbie downer, but gird your loins for the "but now the standard is sublobar resection, so VALOR trial results are not applicable."
I have a fantastic CT surgeon I work with that is busy enough that he doesn't have to try to resect every 1-2 cm NSCLC....but your mileage may vary. There are still ones out there that will do a very risky (anesthesia /lung function wise) wedge over SBRT.
- Joined
- Oct 24, 2010
- Messages
- 3,512
- Reaction score
- 6,365
Biggest issue with ablation is the same reason why biopsies have transitioned from transthoracic CT-guided biopsy to enb biopsies. Pneumothorax rate of 25-50% is no joke and if patients think they weren't given an option for sbrt after they end up in the hospital with a chest tube overnight, well it's going to get out eventually
I've heard of endobronchial ablation as a possibility given increasing electronavigational bronchoscopies but that seems to be more palliative than definitive from what i can tell. Pulmonologists around here aren't sending out for transthoracic biopsies as much here, so not sure why they would all of a sudden start doing more transthoracic ablations 🤷♂️
Report Overview
The global tumor ablation market size was valued at USD 1.14 billion in 2021 and is expected to expand at a compound annual growth rate (CAGR) of 13.5% from 2022 to 2030. The rising prevalence of cancer and the high demand for safer therapeutic options are major factors contributing to the growth of the market. According to the WHO, it is projected that around 10-11 million cancer cases will be diagnosed each year globally by 2030. The number of new cancer cases is expected to increase by more than 80% in low-income countries compared to half the rate in high-income countries (40%) from 2008 to 2030. Lucrative growth potential in currently available therapeutic options and high demand for minimally and non-invasive therapies are the factors expected to drive the market in the upcoming years.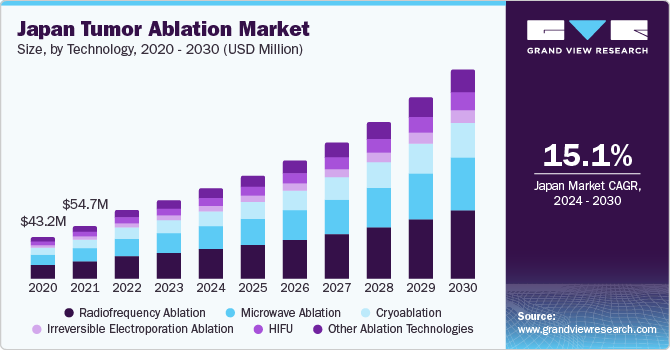
Tumor Ablation Market Size & Share Report, 2030
The global tumor ablation market size was valued at USD 1.14 billion in 2021 and is expected to expand at a compound annual growth rate (CAGR) of 13.5% from 2022 to 2030. The rising prevalence of cancer and the high demand for safer therapeutic options are major factors contributing to the...
 www.grandviewresearch.com
www.grandviewresearch.com
Tumor Ablation Market Size & Share Report, 2030
The global tumor ablation market size was valued at USD 1.14 billion in 2021 and is expected to expand at a compound annual growth rate (CAGR) of 13.5% from 2022 to 2030. The rising prevalence of cancer and the high demand for safer therapeutic options are major factors contributing to the...
Regional Insights
North America dominated the market with a revenue share of over 30.0% in 2021. Major factors contributing to the growth of this region include government support for quality healthcare, high purchasing power parity, the availability of reimbursements, and the increasing prevalence of cancer. For instance, in the U.S., the Patient Protection and Affordable Care Act (PPACA) promotes the quality and affordability of health care through health coverage policies, which reduces the cost of healthcare for individuals and the government. In addition, the precision medicine initiative in formulating tailored strategies for unique characteristics of diseases is a key growth factor. Hence, such government initiatives are anticipated to improve the overall healthcare system, thus boosting market growth.Europe held a considerable revenue share in 2021. A greater extent of public funding in Europe’s healthcare system contributed to this growth. Moreover, the growing geriatric population, coupled with government support to control cancer, is estimated to boost the market growth in this region. For instance, the European Cancer Observatory aims to create awareness about cancer, early diagnostic techniques, and advanced minimally invasive therapeutic options.
Asia Pacific is expected to register the fastest growth rate during the forecast period. Expanding patient population and the growing presence of major healthcare providers in rapidly developing economies such as India and China open growth opportunities. In addition, with government assistance, healthcare utilization in Asia Pacific is improving. For instance, the Indian government provides financial assistance for poor patients suffering from cancer under the Health Minister Cancer Patient Fund (HMCPF) scheme. This is anticipated to fuel the demand for tumor ablation devices in this region over the forecast period.
We can either ignore this “data” and stick with what we are doing or at the very least, start looking around and ask what’s our likely future.
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
Biggest issue with ablation is the same reason why biopsies have transitioned from transthoracic CT-guided biopsy to enb biopsies. Pneumothorax rate of 25-50% is no joke and if patients think they weren't given an option for sbrt after they end up in the hospital with a chest tube overnight, well it's going to get out eventually
I've heard of endobronchial ablation as a possibility given increasing electronavigational bronchoscopies but that seems to be more palliative than definitive from what i can tell. Pulmonologists around here aren't sending out for transthoracic biopsies as much here, so not sure why they would all of a sudden start doing more transthoracic ablations 🤷♂️
Same here.
Our interventional pulm got a robotic bronch with a cone beam ct set up which is a really nice tool. can confirm needle in lesion. The CT guided biopsies have essentially stopped.
THe bigger risk is endobronchial ablation tech IMO.
- Joined
- Sep 20, 2004
- Messages
- 11,743
- Reaction score
- 11,838
Endobronchial HDR has never been curative monotherapy afaik. I see that being in the same bucketSame here.
Our interventional pulm got a robotic bronch with a cone beam ct set up which is a really nice tool. can confirm needle in lesion. The CT guided biopsies have essentially stopped.
THe bigger risk is endobronchial ablation tech IMO.
Surgery is the first-line treatment choice for Stage I NSCLC. For patients who cannot tolerate surgery or who refuse, SBRT is clearly the best second choice. This study changes nothing, given that it's an observational study and only hypothesis-building. VALOR as mentioned above will finally give us good data, hopefully.
I have convinced all our medoncs that, should a patient receive RFA for Stage I NSCLC, they still need to be treated with SBRT, given the unacceptably high recurrence rate with RFA alone.
I have convinced all our medoncs that, should a patient receive RFA for Stage I NSCLC, they still need to be treated with SBRT, given the unacceptably high recurrence rate with RFA alone.
- Joined
- Sep 7, 2014
- Messages
- 3,209
- Reaction score
- 5,916
How many ncdb review based surgery vs sbrt threads are there in this forum now?
- Joined
- Apr 21, 2011
- Messages
- 3,622
- Reaction score
- 9,267
[heads to drew moghanaki's twitter, and waits for brendon stiles to arrive]
NCDB links should have been banned by nowHow many ncdb review based surgery vs sbrt threads are there in this forum now?
Last edited:
- Joined
- Jul 14, 2020
- Messages
- 1,374
- Reaction score
- 4,158
NCDB has been a great boon to many academic careers. The analysis has gotten way too granular and the culture that believes that "there is detailed truth buried in this big data" is frankly scary.
There are lots of broad, general, fairly vague population based truths within the data.
As someone involved in the COC committee at an accredited community hospital, I can speak confidently that the data itself is not robust and not even remotely comparable to the data acquired through typical clinical trials.
There are lots of broad, general, fairly vague population based truths within the data.
As someone involved in the COC committee at an accredited community hospital, I can speak confidently that the data itself is not robust and not even remotely comparable to the data acquired through typical clinical trials.
For endobronchial lesions... that don't extend beyond ~8mm outside the bronchus and are not adjacent to blood vessels. In my practice, this doesn't comprise a meaningful percentage of the patients i seeSame here.
Our interventional pulm got a robotic bronch with a cone beam ct set up which is a really nice tool. can confirm needle in lesion. The CT guided biopsies have essentially stopped.
THe bigger risk is endobronchial ablation tech IMO.
I usually cringe when Drew debates Stiles... but this study deserves a shellacking from DM lol
[heads to drew moghanaki's twitter, and waits for brendon stiles to arrive]
- Joined
- Aug 4, 2020
- Messages
- 1,967
- Reaction score
- 3,354
Sounds like its about as reliable as the VARS data lolNCDB has been a great boon to many academic careers. The analysis has gotten way too granular and the culture that believes that "there is detailed truth buried in this big data" is frankly scary.
There are lots of broad, general, fairly vague population based truths within the data.
As someone involved in the COC committee at an accredited community hospital, I can speak confidently that the data itself is not robust and not even remotely comparable to the data acquired through typical clinical trials.
- Joined
- Oct 10, 2011
- Messages
- 8,624
- Reaction score
- 10,698
NCDB shows surgery is better than radiation. For the 5000th time. Surgeons assume that NCDB accounts for all morbidities and documents them with 100% accuracy.
Jesus ****ing christ.
There are literally 4+ paperson this exact topic already after a 1 minute pubmed search.

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
Can we ****ING STOP
Jesus ****ing christ.
There are literally 4+ paperson this exact topic already after a 1 minute pubmed search.

Comparison of Long-term Survival of Patients With Early-Stage Non-Small Cell Lung Cancer After Surgery vs Stereotactic Body Radiotherapy - PubMed
This study found that, overall, surgery coupled with regional LNE of appropriate extent was associated with the best long-term OS in patients with ES NSCLC.

Survival of Primary Stereotactic Body Radiation Therapy Compared With Surgery for Operable Stage I/II Non-small Cell Lung Cancer - PubMed
Median survival was significantly higher after surgery compared with SBRT in a risk-adjusted matched cohort of patients judged to be surgical candidates. Operable patients considering primary SBRT should be educated regarding this difference in survival.

Lobectomy Versus Stereotactic Body Radiotherapy in Healthy Octogenarians With Stage I Lung Cancer - PubMed
Among healthy octogenarians with clinical stage I NSCLC who are good surgical candidates, lobectomy offers better survival than SBRT. Adequate LN dissection allows true nodal staging and opportunity for adjuvant treatment when unsuspected nodal metastases are found.

Comparative effectiveness of stereotactic body radiation therapy versus surgery for stage I lung cancer in otherwise healthy patients: An instrumental variable analysis - PubMed
In otherwise healthy patients with stage I NSCLC, surgical resection is associated with a survival benefit compared with SBRT. This is true for both lobar and sublobar resections.
Can we ****ING STOP
- Joined
- Oct 24, 2010
- Messages
- 3,512
- Reaction score
- 6,365
You rad oncs and your “data” arguments!
- Joined
- Aug 4, 2020
- Messages
- 1,967
- Reaction score
- 3,354
Wait, now do the lobar versus sublobar long term survival data..


- Joined
- Dec 2, 2011
- Messages
- 1,487
- Reaction score
- 3,011
Comparing survival between focal therapies without any insight into cause specific mortality is pretty close to meaningless. Unless more patients treated with SBRT are dying of lung cancer (which I highly doubt), this study tells us what all of the NCDB prostate studies told us: it is difficult if not impossible to "account" for baseline differences in groups which have vastly different baseline expected survival. Do what you want with the data, but garbage in = garbage out.
- Joined
- Aug 4, 2020
- Messages
- 1,967
- Reaction score
- 3,354
- Joined
- Jun 21, 2022
- Messages
- 944
- Reaction score
- 3,297
I am so sick of this argument and watching the academics (RadOnc and Thoracic surgery) discuss this on Twitter makes me very thankful I left academics.


