- Joined
- Oct 26, 2008
- Messages
- 7,465
- Reaction score
- 4,143
I think this was discussed a while ago but i cant find it. From a non financial point of view and more of a ethical/what's best for the patient. What are you doing for elective cases for patient who tested positive or recently tested positive? Unless this was recently changed, ASA/APSF released joint guideline ages ago recommending delay in order of weeks
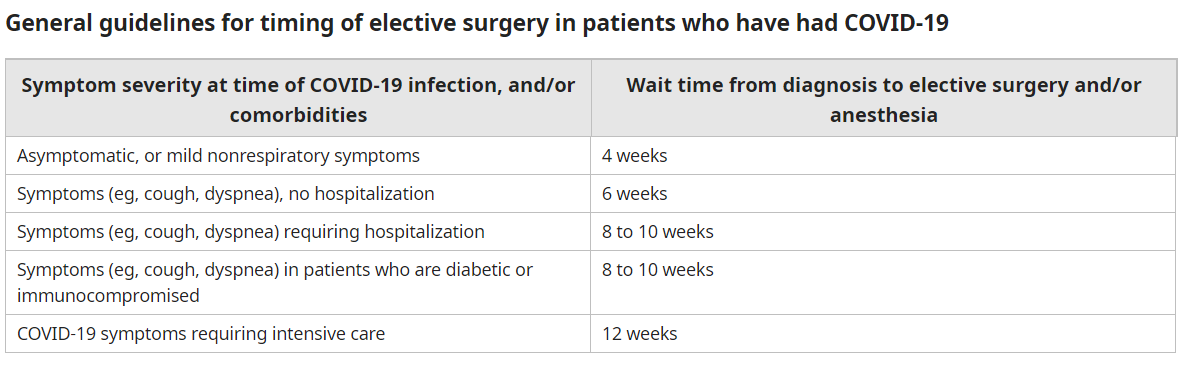
My hospital has a policy of putting covid patients on schedule for surgery only after 10 days after positive test, and 72 hours being asymptomatic.
However this goes directly against ASA/APSF guidelines. This situation kind of feels like if my hospitals NPO policy went against ASA guidelines. Imagine hospital telling patients they can eat full meals up to 2 hours before surgery.
Just to be clear i have no doubt i can get the patient thru surgery so I am not concerned about that. But studies do show way higher mortality post surgery in recent covid+.
"In patients who had been asymptomatic with COVID-19, odds of 30 day mortality after surgery performed within seven weeks of the diagnosis were also increased, but to a lesser extent than patients who had been symptomatic. For surgery performed at zero to two, two to four, and five to six weeks after diagnosis odds ratios were 3.94 (95% CI 2.71-5.17), 3.57 (95% CI 1.96-5.17, and 3.26 (95% CI 1.45-5.07), respectively."
Some have said, just explain to patient the risks, which i guess is one way of doing it. but at the same time if patient showing up for a inguinal hernia ate 2 steaks a hour before surgery, I'm not telling them the risk of aspiration and proceeding... I'm postponing the case
My hospital has a policy of putting covid patients on schedule for surgery only after 10 days after positive test, and 72 hours being asymptomatic.
However this goes directly against ASA/APSF guidelines. This situation kind of feels like if my hospitals NPO policy went against ASA guidelines. Imagine hospital telling patients they can eat full meals up to 2 hours before surgery.
Just to be clear i have no doubt i can get the patient thru surgery so I am not concerned about that. But studies do show way higher mortality post surgery in recent covid+.
"In patients who had been asymptomatic with COVID-19, odds of 30 day mortality after surgery performed within seven weeks of the diagnosis were also increased, but to a lesser extent than patients who had been symptomatic. For surgery performed at zero to two, two to four, and five to six weeks after diagnosis odds ratios were 3.94 (95% CI 2.71-5.17), 3.57 (95% CI 1.96-5.17, and 3.26 (95% CI 1.45-5.07), respectively."
Some have said, just explain to patient the risks, which i guess is one way of doing it. but at the same time if patient showing up for a inguinal hernia ate 2 steaks a hour before surgery, I'm not telling them the risk of aspiration and proceeding... I'm postponing the case