- Joined
- Apr 1, 2007
- Messages
- 295
- Reaction score
- 55
hey guys, just a quick case just wondering what you guys think..
pt is scheduled for TEE/RHC by the cardiologist and you are asked to provide anesthesia.
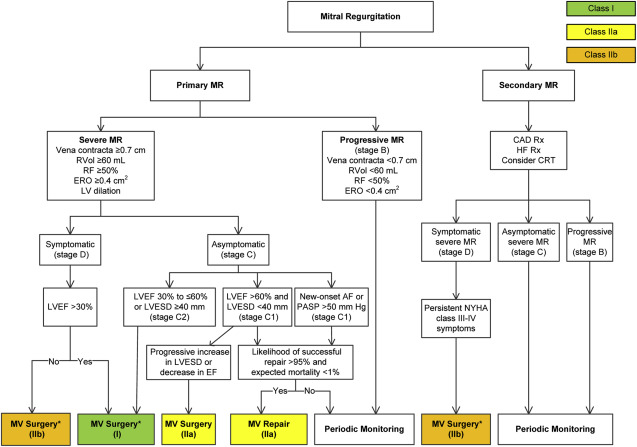
37 yo F with coronary artery vasospasm: s/p LHC on 5/13 with 90% narrowing of the LAD. staged PCI revealed normal coronaries. acute systolic CHF: Patient in respiratory distress with bilateral crackles on exam. chest x-ray on 05/18 revealed new interstitial pulmonary edema. chest x-ray on 5/20 shows worsening infiltrates and/or edema. TTE on 5/14 revealed mildly increased LV wall thickness with normal systolic function and estimated LVEF 55-60%. TTE on 5/18 revealed LVEF 35-45% with akinesis of basal-mid inferior lateral myocardium with severe MR (possible ruptured chordae),
RVSP=31mmHg
she is currently tachycardic in the 120s and hypotensive with blood pressure ranging in 80s-90/50s-60s with s/s of acute respiratory failure on oximyzer 11 LPM most likely cardiogenic pulm edema from acute CHF.
obviously i'm concerned about cardiopulmonary/hemodynamic decompensation so..
would you consider telling the cardiologist to spray some topical lido and give a touch of midaz/fentanyl and give it a go?
touch of prop/versed/fent/ketamine?
cancel?
CT surgery?
pt is scheduled for TEE/RHC by the cardiologist and you are asked to provide anesthesia.
37 yo F with coronary artery vasospasm: s/p LHC on 5/13 with 90% narrowing of the LAD. staged PCI revealed normal coronaries. acute systolic CHF: Patient in respiratory distress with bilateral crackles on exam. chest x-ray on 05/18 revealed new interstitial pulmonary edema. chest x-ray on 5/20 shows worsening infiltrates and/or edema. TTE on 5/14 revealed mildly increased LV wall thickness with normal systolic function and estimated LVEF 55-60%. TTE on 5/18 revealed LVEF 35-45% with akinesis of basal-mid inferior lateral myocardium with severe MR (possible ruptured chordae),
RVSP=31mmHg
she is currently tachycardic in the 120s and hypotensive with blood pressure ranging in 80s-90/50s-60s with s/s of acute respiratory failure on oximyzer 11 LPM most likely cardiogenic pulm edema from acute CHF.
obviously i'm concerned about cardiopulmonary/hemodynamic decompensation so..
would you consider telling the cardiologist to spray some topical lido and give a touch of midaz/fentanyl and give it a go?
touch of prop/versed/fent/ketamine?
cancel?
CT surgery?