- Joined
- May 7, 2014
- Messages
- 1,657
- Reaction score
- 3,473
A smaller pool of patients compared to a decade ago or longer, given the higher number of pts choosing active surveillance, coupled with PCPs performing less PSA screening after the USPTF recs against it several years ago (although this did change very recently).Maybe a naive question, but might SBRT result in higher proportion of patients selecting radiation therapy over RP, with this at least partially offsetting the decrease in # of fractions?
I have been here all along. My default regimen brachy for appropriate patients; otherwise 60/20 or for selected patients SBRT.Where have you been? Hypofrac and Sbrt are the future. There’s no turning back from this stuff. Gonna work its way into literally every disease site they can get enough data for. Only hope is APMs that way we can hypofrac the living daylights out of everything we can get away with. Until then You just need to hope your employer doesn’t fire you when your Dept’s revenue drops off a cliff. But hey we’re in such high demand these days...right? We’ll land on our collective feet...
Maybe a naive question, but might SBRT result in higher proportion of patients selecting radiation therapy over RP, with this at least partially offsetting the decrease in # of fractions?
In my practice, over 50% of my patients are hypofractionationed in some way, either SRS, 1-5 fraction SBRT/FSRT, or 1-5 fraction palliative cases. I never have more than 15 on beam, and my RVUs are solid for academics. This is the future.
Maybe a naive question, but might SBRT result in higher proportion of patients selecting radiation therapy over RP, with this at least partially offsetting the decrease in # of fractions?
I doubt that SBRT will suddenly lead to a lot more men choosing radiation over RALP. In many parts of the country, men with prostate cancer never even have a consultation with a RO. Urologists own the patients and they can be quite effective at scaring patients away from the "harms" of radiation.
Many of the aggressive/unscrupulous urologists are going to jump on HIFU, whole gland or focal, to avoid sending nonsurgical pts for XRT, just like many have and, in some cases, continue to do cryosurgery inappropriately for upfront therapyI agree that this is an issue for many practices, no doubt. But as sbrt becomes more widely adopted and becomes commonly known, it’s going to be harder for urologists to downsell it. Kind of a long game win.
Also you’re still seeing some patients wirh intact prostate I’m sure - are these JUST patients that aren’t medically operable?
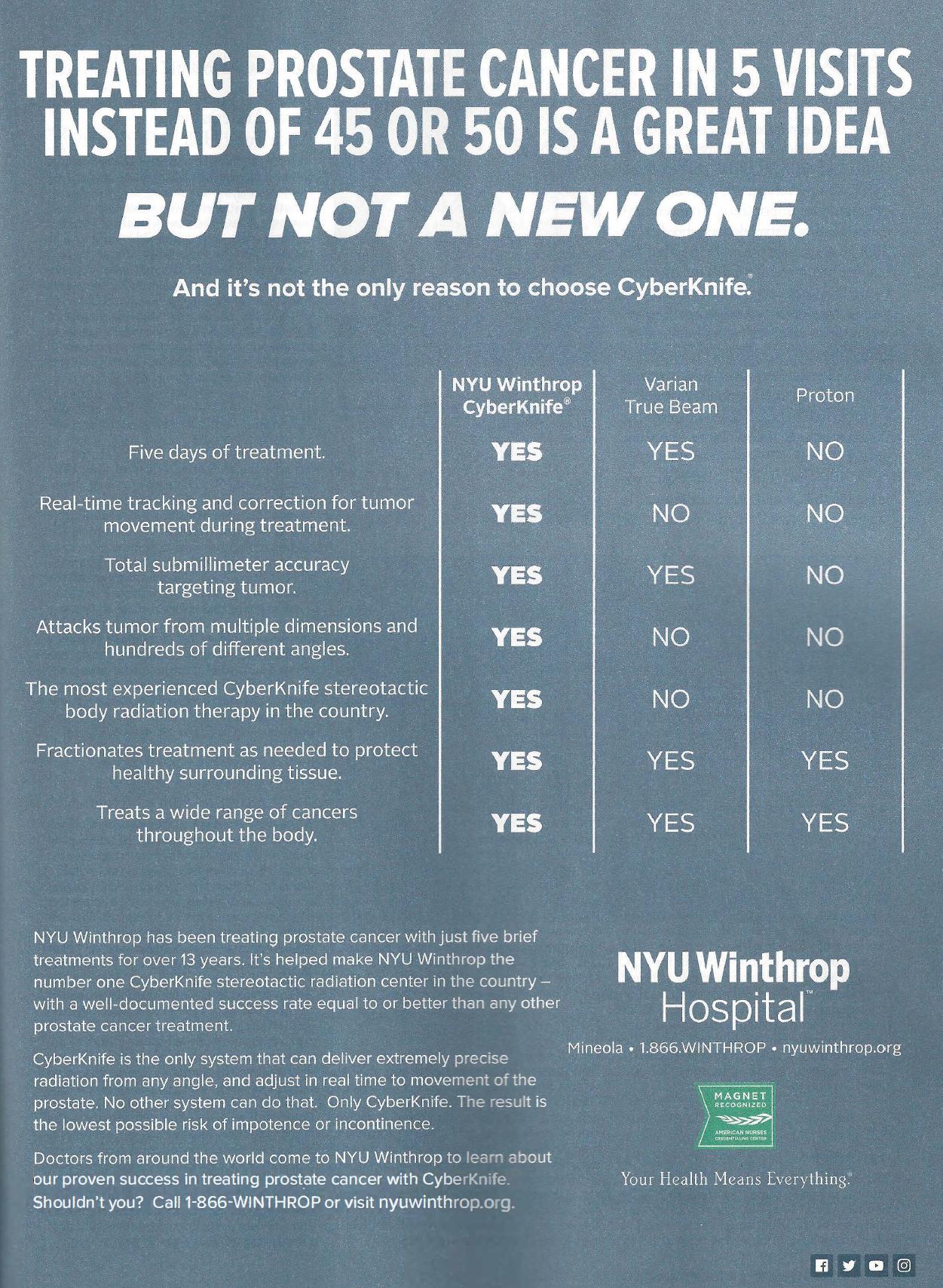
Must be a real long game kid. As I was eating caviar last night I noticed this ad was in my "The New Yorker." I have seen roadside billboards in Florida advertising the same "breakthroughs" for twenty years. Know what that's got us? Bupkis! Once I figure out how to diagnose prostate cancer all on my wonderful own, I can control the patient. That's why I'm advocating that we become interventional radiologists AND rad oncs, you see...I agree that this is an issue for many practices, no doubt. But as sbrt becomes more widely adopted and becomes commonly known, it’s going to be harder for urologists to downsell it. Kind of a long game win.
Also you’re still seeing some patients wirh intact prostate I’m sure - are these JUST patients that aren’t medically operable?
ASTRO, at one point a few years ago, looked into trying to have CMS split imrt into simple (prostate) and (complex). It's crazy to me that a prostate only ebrt plan reimburses the same planning charge as a head and neck or pelvic imrt planI would humbly submit that the problem is the *****ic way institutions/people are reimbursed per fraction instead of per course. Once this is taken into proper perspective, there will be no impediment to hypofractionate everything and suddenly people will have an "awakening."
Can anyone honestly tell me why a 41 fraction prostate cancer VMAT course should reimburse more than a 10-20 fraction lymphoma VMAT case? The stakes are way higher with the latter, not to mention the risk of secondary malignancy which is germane in 30-40 year old patients and not in 70-80 year old low-risk prostate patients.
I would humbly submit that the problem is the *****ic way institutions/people are reimbursed per fraction instead of per course. Once this is taken into proper perspective, there will be no impediment to hypofractionate everything and suddenly people will have an "awakening."
Can anyone honestly tell me why a 41 fraction prostate cancer VMAT course should reimburse more than a 10-20 fraction lymphoma VMAT case? The stakes are way higher with the latter, not to mention the risk of secondary malignancy which is germane in 30-40 year old patients and not in 70-80 year old low-risk prostate patients.
Perhaps in the case of bone mets:
Reimburse a flat fee for planning and the first 5 fractions. Every additional fraction will also be reimbursed but with a significantly lower amount per fraction as of what is being reimbursed today. That way you are discouraging physicians from "overfractionating".
Reimburse VMAT or SBRT only if certain parameters are met (good PS, favorable prognosis, pretreatment).
I doubt that SBRT will suddenly lead to a lot more men choosing radiation over RALP. In many parts of the country, men with prostate cancer never even have a consultation with a RO. Urologists own the patients and they can be quite effective at scaring patients away from the "harms" of radiation.
At least the younger ones operate. The old timers will cryoablate whole gland or "focal", while some of them would even fly cash patients out to the islands or Mexico for HIFUAggressive group of urologists in my area -- all young, <10 years out from training, and operate on everyone. No qualms about saying "patient refused radiation" in Tumor Board discussions. THEY'RE the ones talking to patients about radiation, and in vast majority of cases, deter them from it. I'll never get used to it, this idea that no patients are truly "our" patients, that we just get to borrow them a few weeks. Uros get away with it all the time, at least where I am. It devalues our expertise and training, and gyps the patient of an opportunity to hear expert opinion about all of their options, and then making an informed decision that's best for them. I'm trying to get the PCPs to refer every patient with prostate cancer to both urologist and radonc, but it's in one ear/out the other.
Is that not 77385 and 77386.ASTRO, at one point a few years ago, looked into trying to have CMS split imrt into simple (prostate) and (complex).
A 3D course of tx at 35 fractions is about $14,000. So let's assume a complex tx (custom blocking, tangents, wedges, etc., ie 3D). If each "3D fraction" goes for about $275, then ROUGHLY....Does anyone know the cost difference for a 5 or 10 fraction course vs. a 20 fraction course? The difference between 10 and 20 fractions is certainly not double.
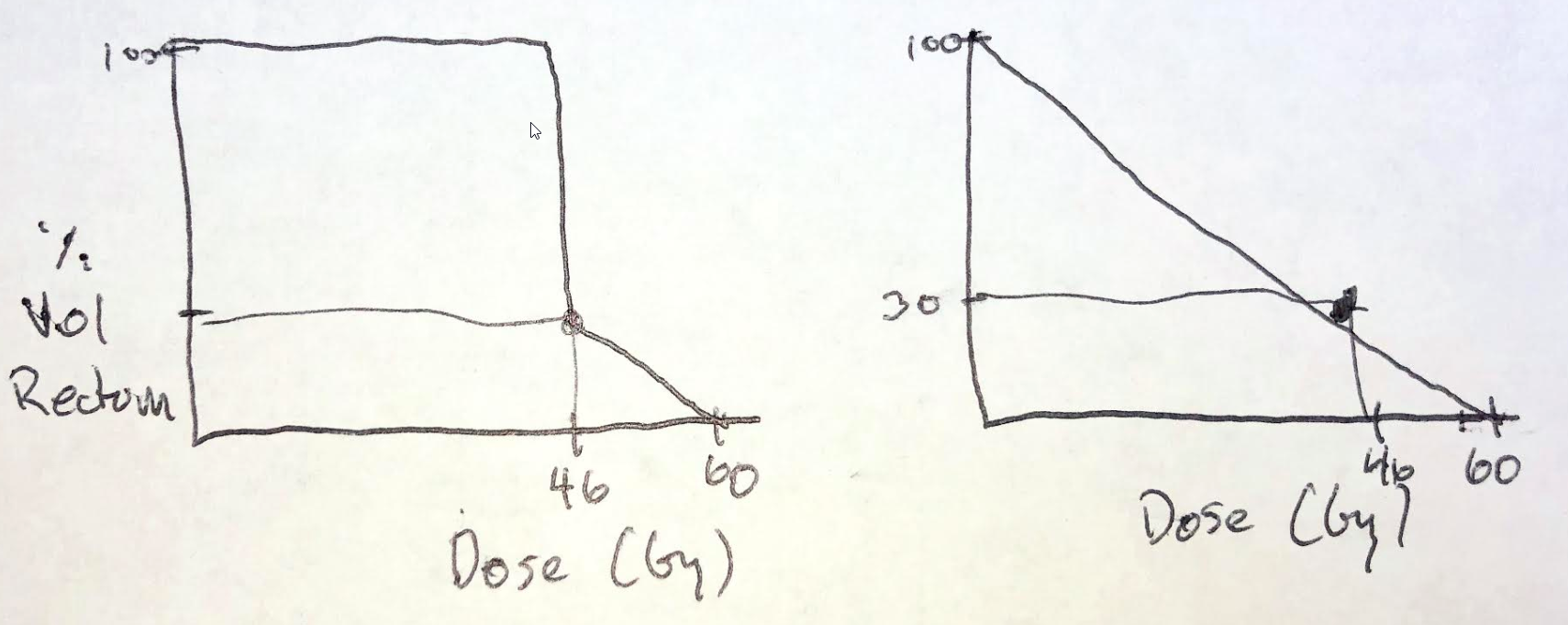
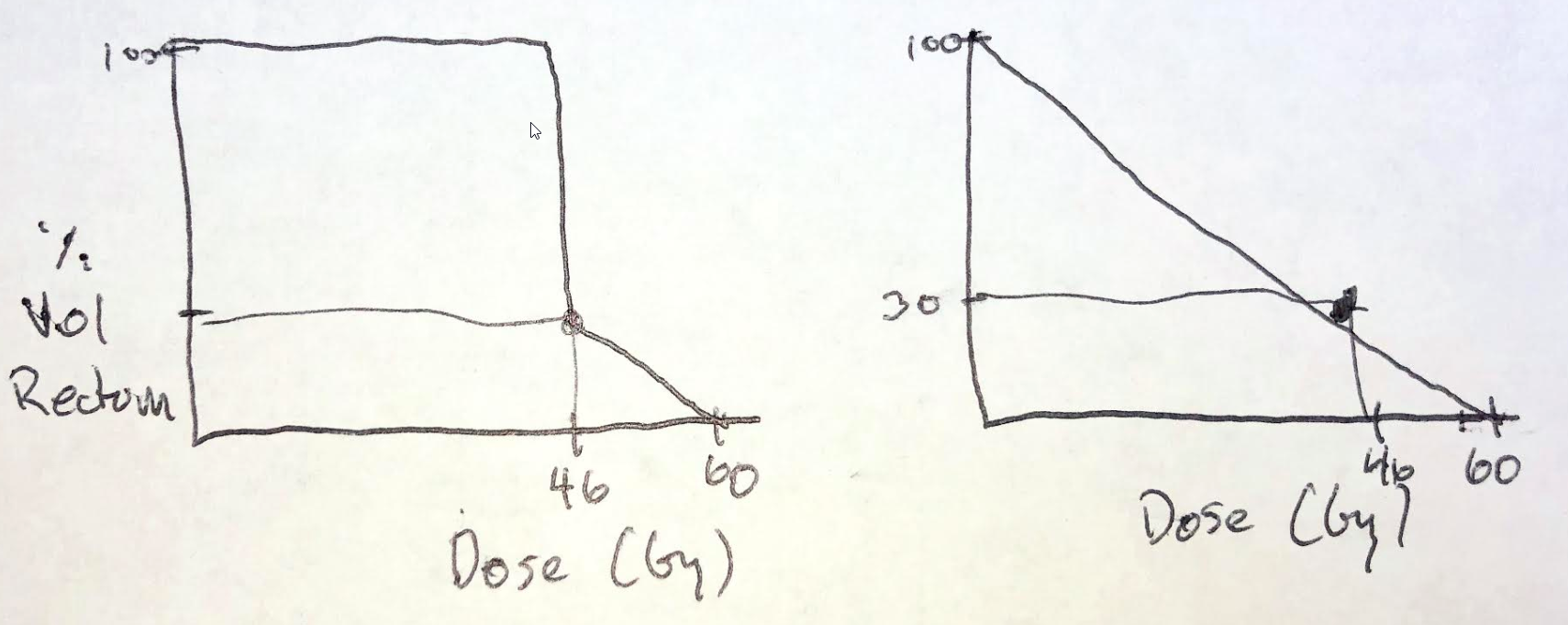
One would assume keep 70% or more of rectum ("<Vol%") to 46Gy or less e.g. One would assume. What's dumb about constraints is that both of these DVHs below meet the rectal constraints. (They did add in a 50% 37 Gy constraint, even so...) But which curve would you want???Speaking of prostate hypofractionation... I was reading the "ASTRO, ASCO, and AUA Evidence-Based Guideline"
https://ascopubs.org/doi/full/10.1200/JCO.18.01097
Can someone tell me how this works?
View attachment 257294
I was under the impression that with rising dose less % of the OAR should receive that dose...

I was referring to 77301. Tx planning, not delivery. I think ASTRO was trying to target urorads with that oneIs that not 77385 and 77386.
I once heard Nancy Lee say it took her a few hours to do an NPC case. Whew! Maybe we should do like lawyers and charge patients for billable hours spent contouring/planning. That'd be the most honest way... if everyone was honest. The way human nature is, we would probably see a study on improved clinical outcomes with time spent contouring. Still, some rad oncs are fast and some slow in various clinical scenarios; it can take me longer on a prostate than a H&N sometimes. Regardless, I like to be speedy. I like to approach planning and contouring like the surgeons of old, "Time me, gentlemen."I was referring to 77301. Tx planning, not delivery. I think ASTRO was trying to target urorads with that one
I would humbly submit that the problem is the *****ic way institutions/people are reimbursed per fraction instead of per course. Once this is taken into proper perspective, there will be no impediment to hypofractionate everything and suddenly people will have an "awakening."
Can anyone honestly tell me why a 41 fraction prostate cancer VMAT course should reimburse more than a 10-20 fraction lymphoma VMAT case? The stakes are way higher with the latter, not to mention the risk of secondary malignancy which is germane in 30-40 year old patients and not in 70-80 year old low-risk prostate patients.
Protons were supposed to be better, given the significant cost differential, while hypofx costs the system less."Hypofractionation is non-inferior to standard fractionation and thus should be the new standard of care"
"Proton therapy is non-inferior to photon therapy and thus should be the new standard of care"
I cant imagine they are shameless enough to say that about protons and was pleasantly surprised to see the oped in JCO trashing protons for lung ca (and rightfully so)
So you agree with me that their constraints make no sense whatsoever?One would assume keep 70% or more of rectum ("<Vol%") to 46Gy or less e.g. One would assume. What's dumb about constraints is that both of these DVHs below meet the rectal constraints. (They did add in a 50% 37 Gy constraint, even so...) But which curve would you want???
Would the following sound better?Speaking of prostate hypofractionation... I was reading the "ASTRO, ASCO, and AUA Evidence-Based Guideline"
https://ascopubs.org/doi/full/10.1200/JCO.18.01097
Can someone tell me how this works?
View attachment 257294
I was under the impression that with rising dose less % of the OAR should receive that dose...
First I thought it was a typo in the JCO paper. But it seems the trial protocol was actually written that way...
https://ascopubs.org/doi/suppl/10.1200/JCO.2016.71.7397/suppl_file/protocol_2016.717397.pdf
View attachment 257295
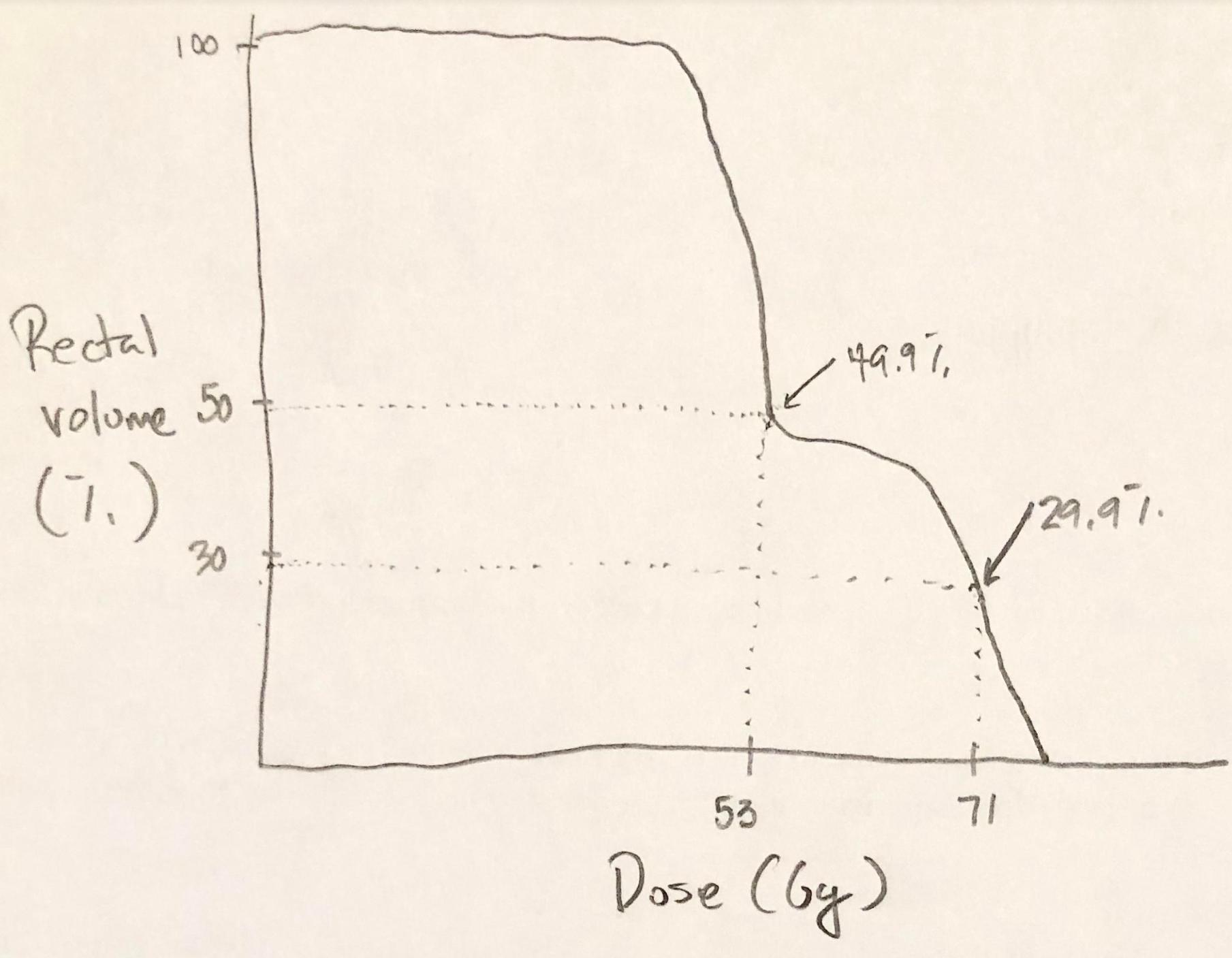
Would the following sound better?
71 Gy to no more than 30%
53 Gy to no more than 50%
Both are saying the same thing. (I think; but I sure that the misanthropes and deplorable of SDN will correct me)
The popular constraint of 70 Gy <25% of rectum is the same as 75% of rectum to receive less than 71 Gy; right?
This horrible rectal DVH curve meets those reasonable sounding criteria.Would the following sound better?
71 Gy to no more than 30%
53 Gy to no more than 50%
Yes, but you know that a competent radiation oncologist would not sign that plan because while meeting the constraints a competent radiation oncologist would know that it is possible to derive a better solution.
I have seen many situations where people "met literature constraints" yet generated DVHs which could have been easily improved. While we don't write out DVHs per se, we birth DVHs with constraints as starting points. Looking at the prostate literature and the table Palex80 posted above, I have made better DVHs in 100% of cases than what the literature constraints allow. 100%. Which means the literature constraints allow for DVHs (and clinical outcomes probably) which are worse than achievable. That ain't good. The (prostate rectal) constraints are superfluous paper tigers. There have been attempts to create different ways of conveying constraints versus one or two thou-shall-not-pass points on a DVH; they've not gained traction. Although it matters how close a DVH constraint point is to the Rx dose. Again in the table above where all doses are prescribed at about 60-70 Gy, I don't see a point constraint at ~33% of the Rx dose, ie at 20 Gy. In stage III lung planning where have Rx doses to 60+ Gy, we care a lot about a DVH point at 20 Gy to a particular OAR. That makes optimization harder, which is good. If DVH point constraints are set closer to the Rx dose for an OAR, it makes optimization easier, which is bad. All the rectal constraints above, save Fox Chase's (who have constraint points farthest from the Rx dose... they have a point at ~42% of Rx dose), allow for rectal doses which I never have/never will countenance and set up for IMRT optimizations with little-to-no cost, mathematically speaking.By that metric, tons and tons of Bad DVHs could be written out for almost any constraint.
This horrible rectal DVH curve meets those reasonable sounding criteria.
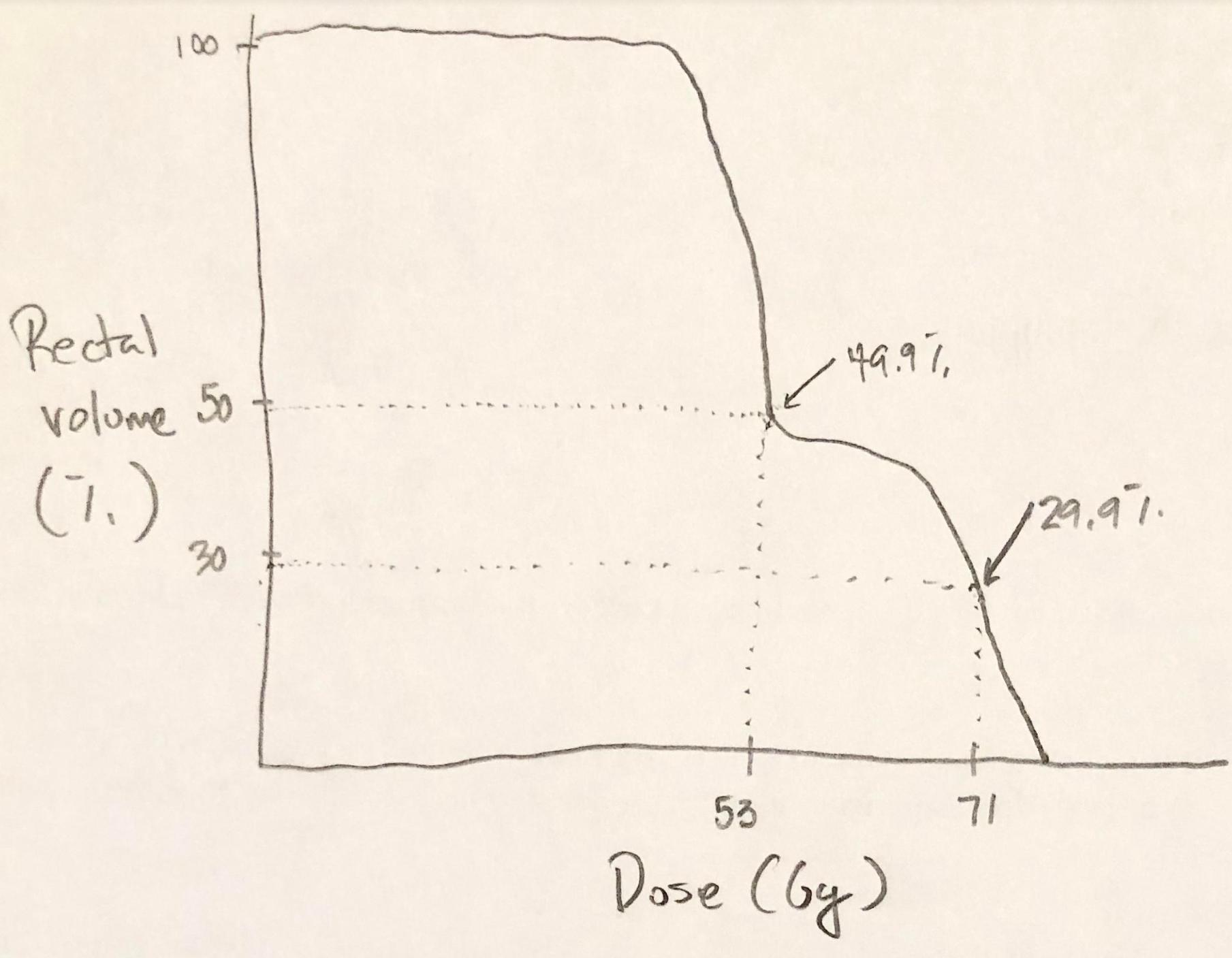
The point I was trying to make is that those DVH constraints make no sense... Irrelevant if you look at the JCO paper or the protocol, they make no sense.
If you demand that less than 50% of the rectal wall should receive 37 Gy, what's the point in saying that less than 70% of the rectal wall should receive 46 Gy?
In other words the constraints say:
V37 < 50% and V46 < 70%
View attachment 257454
That makes no sense.
The DVH would have to climb rather than fall to meet that constraint.
I do on all my pelvic and h&n imrt pts.... 0.5-0.7 cm. How many of us are routinely putting PTV margins on all of our contoured lymph node regions and evaluating plans/DVHs based on that? Maybe I'm an outlier but I don't do that in routine clinical practice.
I do on all my pelvic and h&n imrt pts.... 0.5-0.7 cm
The constraints on this table don't say anything clinically helpful and are vague and there is no standardized lingo AMAZINGLY (obviously!) in radiation oncology for constraint conveyance without getting wordy and/or using mathematical inequality operators everywhere (e.g. ≤ or ≥). Highly recommend the latter versus the former. All these constraints say is "37 Gy, <Vol% 50%... 46Gy, <Vol% 70." What the heck is "less than volume percent"??? Is one percent "<Vol% 70"? Sure. So 49% of the rectum ("<Vol% 50") could get 37Gy or more, and 1% of the rectum ("<Vol% 70") could get 46Gy or more. Constraint met, DVH falling not rising, nice DVH curve. (69% is also "<Vol% 70," and if you went there, yeah, the DVH would rise not fall.)If you demand that less than 50% of the rectal wall should receive 37 Gy, what's the point in saying that less than 70% of the rectal wall should receive 46 Gy?
In other words the constraints say:
V37 < 50% and V46 < 70%
That makes no sense.
The DVH would have to climb rather than fall to meet that constraint.
Which is, in fact, my ultimate point for "almost any poorly specified constraint."what a ridiculous hypothetical proposed by scarbrtj. By that metric, tons and tons of Bad DVHs could be written out for almost any constraint.
Chartreuse's point is that it's actually NOT saying V37 < 50% and V46 < 70%.
That is how I initially read it as well, but it's likely a misquoting of the PROFIT protocol (based on the picture you had earlier of how they phrase their constraints).
The proper way I would phrase that constraint would essentially be V37 < (100-50%) = V37 < 50% and V46 < (100-70%) = V46 < 30%, which is more in line with what CHHiP has.
And don't even get me started on the RTOG 0415 constraints, which I've tried to use previously when treating with 70/28. Prescription dose is 70Gy and your Rectal constraint is V74 < 15%? Such lazy trial and constraint writing to literally just copy and paste from the standard fractionation arm without thought on what an appropriate constraint would be.
Is anyone aware of any published, reasonable constraints for 70/28 (as my institutions most common prostate hypofrac regimens) ? Ideally ones that have some actual dose-respondent toxicity outcomes correlated to them?
Thanks. Link to article this is from (if possible)? Would like to have a paper to give to attendings/dosimetrists rather than just saying some guy on the internet sent me this.
I do. We had that argument before.Also, sometimes people do things differently in clinical practice than they do for the trial. For example, NSABP-B51 mandates PTV margins (I believe 5mm) for all the lymph node basins and evaluation of coverage based on that. How many of us are routinely putting PTV margins on all of our contoured lymph node regions (EDIT - in breast cancer patients) and evaluating plans/DVHs based on that? Maybe I'm an outlier but I don't do that in routine clinical practice.
