- Joined
- Nov 28, 2016
- Messages
- 159
- Reaction score
- 160
Let me preface this by saying I am 100% about empiricism. I was trained hardcore in evidence-based practices, the importance of research informed therapy, and to be a good consumer/critic of research. I currently use CBT, ACT, and exposure and response prevention as my main modalities. So...don't get too angry. I want you all to think about something though. The Contextual model of psychotherapy proposed in The Great Psychotherapy Debate by Wampold and Imel (a freaking MUST read) provides a **** ton of evidence that change doesn't happen in psychotherapy like it does in medical treatments. In medicine, you have high blood pressure, you take propanolol, blood pressure reduces, you're good to go. However, with therapy change seems to happen when 4 criteria are met: 1. There is a good therapeutic alliance. 2. Empathetic and caring therapist who believes the treatment will work 3. Some sort of psychologically valid explanation of the client's problem is given, which is culturally acceptable and the client believes (creating hope and expectation). 4. The client engages in SOME sort of healthy behavior change (it doesn't matter exactly what they do). He shows that it doesn't matter what you do or how you do it...as long as it meets these criteria. He provides a rational for why this works (e.g. placebo effect and evolutionary history of humans healing within a social context), but you can read for more details on this.
When you browse through the literature and see how every bonified (i.e. established, widely used, evidence based intervention) therapy is basically the same effectiveness for almost every disorder. I HATE this....I hate how a recent study showed EMDR was as effective as ERP in treating OCD (like WTF...I cited this at the end*), Let me get this straight...it's not saying you can just chat with a client and expect change, but as long as those 4 criteria are met people can't help but get better. Whether its ERP, EMDR, brainspotting, emotion-focused, ISTDP, etc. People will argue that the so called "dodo bird hypothesis" is wrong for various reasons. Do your due diligence and read up on both sides, but Wampold's arguments are solid and grounded in so many studies.
Cognitive therapy seems much more legit than EMDR...but how do we know that cognitive restructuring is affecting change by re-shaping information processing systems, when behavioral activation with no cognitive re-structuring works, increased exercise works, interpersonal therapy works, and psychodynamic therapy works, etc. It's annoying that EMDR is so glaringly in your face about how the eye movements don't make sense, but it has helped thousands of people. Maybe the eye part helps people buy into trauma treatment that wouldn't otherwise receive treatment? I believe we NEED evidence-based practices as vehicles to deliver the components of treatment that work (and to know what doesn't work), but i'm not sure it matters exactly what we do as long as we follow those guidelines.
Feel free to rip apart any of what I said. I'm a nerd about this stuff and enjoy seeing things from new perspectives. I LOVE evidence-based practices, but the evidence for the contextual model/common factors seem undeniable. Please remember Wampold is NOT saying "common factors" like a good relationship and positive regard will cure any psychological ailment. There has to be a valid therapeutic ritual, and positive behavior change. Also, check out the article below for a great review of the Contextual Model and current state of the literature. TLDR: We've been doing psychological research for 50 years and still don't know how therapy works.
Cuijpers, P., Reijnders, M., & Huibers, M. J. (2019). The role of common factors in psychotherapy outcomes. Annual Review of Clinical Psychology, 15, 207-231.
Bonus points if you can rip the below study apart and tell me how EMDR matched CBT for OCD
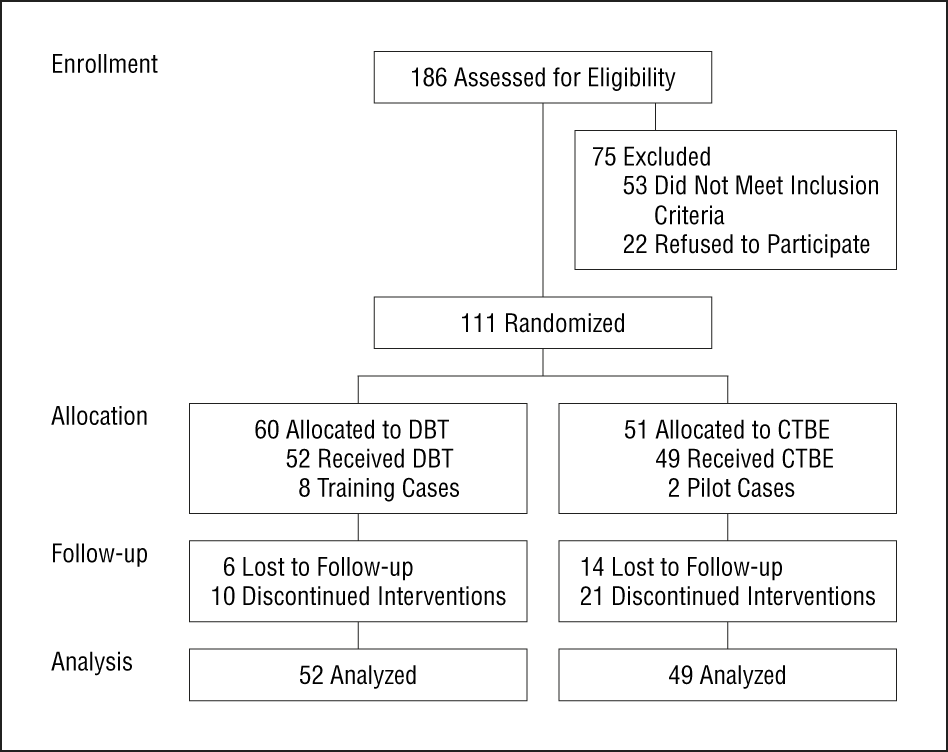
* Marsden, Z., Lovell, K., Blore, D., Ali, S., & Delgadillo, J. (2018). A randomized controlled trial comparing EMDR and CBT for obsessive–compulsive disorder. Clinical psychology & psychotherapy, 25(1), e10-e18.
When you browse through the literature and see how every bonified (i.e. established, widely used, evidence based intervention) therapy is basically the same effectiveness for almost every disorder. I HATE this....I hate how a recent study showed EMDR was as effective as ERP in treating OCD (like WTF...I cited this at the end*), Let me get this straight...it's not saying you can just chat with a client and expect change, but as long as those 4 criteria are met people can't help but get better. Whether its ERP, EMDR, brainspotting, emotion-focused, ISTDP, etc. People will argue that the so called "dodo bird hypothesis" is wrong for various reasons. Do your due diligence and read up on both sides, but Wampold's arguments are solid and grounded in so many studies.
Cognitive therapy seems much more legit than EMDR...but how do we know that cognitive restructuring is affecting change by re-shaping information processing systems, when behavioral activation with no cognitive re-structuring works, increased exercise works, interpersonal therapy works, and psychodynamic therapy works, etc. It's annoying that EMDR is so glaringly in your face about how the eye movements don't make sense, but it has helped thousands of people. Maybe the eye part helps people buy into trauma treatment that wouldn't otherwise receive treatment? I believe we NEED evidence-based practices as vehicles to deliver the components of treatment that work (and to know what doesn't work), but i'm not sure it matters exactly what we do as long as we follow those guidelines.
Feel free to rip apart any of what I said. I'm a nerd about this stuff and enjoy seeing things from new perspectives. I LOVE evidence-based practices, but the evidence for the contextual model/common factors seem undeniable. Please remember Wampold is NOT saying "common factors" like a good relationship and positive regard will cure any psychological ailment. There has to be a valid therapeutic ritual, and positive behavior change. Also, check out the article below for a great review of the Contextual Model and current state of the literature. TLDR: We've been doing psychological research for 50 years and still don't know how therapy works.
Cuijpers, P., Reijnders, M., & Huibers, M. J. (2019). The role of common factors in psychotherapy outcomes. Annual Review of Clinical Psychology, 15, 207-231.
Bonus points if you can rip the below study apart and tell me how EMDR matched CBT for OCD
* Marsden, Z., Lovell, K., Blore, D., Ali, S., & Delgadillo, J. (2018). A randomized controlled trial comparing EMDR and CBT for obsessive–compulsive disorder. Clinical psychology & psychotherapy, 25(1), e10-e18.