Hey all, EM trainee here, had a sick patient in small community ED with DKA BS600s, bicarb 8, AG 28, pH 7.2 on VBG and vitals normal (sx for over a week, compensated fairly well). No big deal except K was 2.8. 2 large bore peripheral IVs, started peripheral K infusion at 10meq/hr and PO 40meq, talked to ED pharmacy who said we could go up to 20meq/hr divided by both IVs... we rechecked in an hour and K was still like 2.9. At this point we just called for transfer to bigger local hospital ICU that was staffed by hospitalist, who chewed me out for not replacing K faster thereby delaying the insulin gtt, and said I should double it to 20meq/hr in each IV, aka total 40meq/hr. It was too busy for us to place central line but he said it was fine peripherally for a critical patient, short term, monitored, etc. I've never heard this before and it seemed like too much to me. Tried to do some research and I don't see much on this out there. Thoughts?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Thoughts on severe DKA with hypokalemia case?
- Thread starter EMgordo
- Start date
- Joined
- Jul 28, 2014
- Messages
- 5,513
- Reaction score
- 9,518
Stupid question but did you check the Mg?
- Joined
- Jul 28, 2014
- Messages
- 5,513
- Reaction score
- 9,518
From a quick search:
IV Infusion
Administration of potassium-containing infusions must be by slow intravenous infusion, including boluses of potassium for hypokalemia (rate of administration generally should not exceed 20 mEq/hour). When including potassium in the long term or maintenance fluid administration, concentration should not exceed 40 mEq/L (exceptions may be severe hypokalemia associated with cardiac arrhythmias or diabetic ketoacidosis where higher concentrations of 60 to 80 mEq/L require caution). Continuous ECG monitoring and serial measurements of plasma potassium concentrations are essential during IV administration of potassium, particularly when the rate of administration is greater than 20 mEq/hour.
Potassium IV solutions should be administered only in well-hydrated patients and with adequate urine flow (especially in post-surgical patients).
The selection of potassium dosages requires caution in patients with renal impairment and geriatric patients.[8]
Potassium acetate, potassium chloride, and potassium phosphate are available as concentrated solutions that require dilution before intravenous administration. Local vascular intolerance may be a limiting factor in the ability to administer concentrated solutions. Ideally, potassium infusion administration should be via a large, high-flow vein (e.g., femoral vein), or administration of solutions of lower concentration may be in divided doses via peripheral veins.
IV Infusion
Administration of potassium-containing infusions must be by slow intravenous infusion, including boluses of potassium for hypokalemia (rate of administration generally should not exceed 20 mEq/hour). When including potassium in the long term or maintenance fluid administration, concentration should not exceed 40 mEq/L (exceptions may be severe hypokalemia associated with cardiac arrhythmias or diabetic ketoacidosis where higher concentrations of 60 to 80 mEq/L require caution). Continuous ECG monitoring and serial measurements of plasma potassium concentrations are essential during IV administration of potassium, particularly when the rate of administration is greater than 20 mEq/hour.
Potassium IV solutions should be administered only in well-hydrated patients and with adequate urine flow (especially in post-surgical patients).
The selection of potassium dosages requires caution in patients with renal impairment and geriatric patients.[8]
Potassium acetate, potassium chloride, and potassium phosphate are available as concentrated solutions that require dilution before intravenous administration. Local vascular intolerance may be a limiting factor in the ability to administer concentrated solutions. Ideally, potassium infusion administration should be via a large, high-flow vein (e.g., femoral vein), or administration of solutions of lower concentration may be in divided doses via peripheral veins.
Potassium - StatPearls - NCBI Bookshelf
www.ncbi.nlm.nih.gov
- Joined
- Aug 10, 2011
- Messages
- 251
- Reaction score
- 194
Patient definitely needs massive hydration too; all good points above. CVL would be optimal, but large bore IVs in a pinch. Bolus 4 liters of LR and give 2-4 gm Mg empirically; start K at 20 men per hour and insulin .08-.1 U/.kg bolus; and keep going with the LR!
- Joined
- Sep 27, 2008
- Messages
- 3,015
- Reaction score
- 2,223
That guy sounds like a douche, I wouldn't worry about it.
Patient doesn't sound that sick honestly, probably at higher risk from iatrogenesis than DKA in the immediate term. Unless the pt had terrible EKG changes or looked like he was about to die, I would just 40 meq PO x2 and 10-20 meq/hr IV and recheck it in a few hours then start the insulin.
I guess you could try to get clever and rapidly replete at 40-60 meq/hr IV along w/ an insulin drip to force it all intracellularly, but the logistics of it make my head spin and you run a non-zero chance of causing the patients myocytes to fibrillate. Especially in a small hospital.
Patient doesn't sound that sick honestly, probably at higher risk from iatrogenesis than DKA in the immediate term. Unless the pt had terrible EKG changes or looked like he was about to die, I would just 40 meq PO x2 and 10-20 meq/hr IV and recheck it in a few hours then start the insulin.
I guess you could try to get clever and rapidly replete at 40-60 meq/hr IV along w/ an insulin drip to force it all intracellularly, but the logistics of it make my head spin and you run a non-zero chance of causing the patients myocytes to fibrillate. Especially in a small hospital.
- Joined
- Feb 27, 2015
- Messages
- 2,265
- Reaction score
- 4,222
Big vein, it'll be fine until you can place a central line. But why? This patient is not that sick and will get better. I wouldn't call a potassium of 2.9 "critical." I think you did fine, and I think the hospitalist was being obnoxious.
I agree with lots of LR and giving IV Mg upfront.
In more rural areas without good nursing support, I often treat mild-moderate DKA with subcutaneous insulin using the Umpierrez protocol. Works really well. Lots of dogma around DKA.

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
I agree with lots of LR and giving IV Mg upfront.
In more rural areas without good nursing support, I often treat mild-moderate DKA with subcutaneous insulin using the Umpierrez protocol. Works really well. Lots of dogma around DKA.

Treatment of diabetic ketoacidosis with subcutaneous insulin aspart - PubMed
Our results indicate that the use of subcutaneous insulin aspart every 1 or 2 h represents a safe and effective alternative to the use of intravenous regular insulin in the management of patients with uncomplicated DKA.
Last edited:
- Joined
- Oct 10, 2007
- Messages
- 4,253
- Reaction score
- 7,081
Yea ph 7.2 is DKA in great shape. When they get under 7 I consider them on the sicker side though most of them still look ok at a glance even though their PCO2 is <10. No arrhythmias and not on the verge of respiratory collapse no reason to push K in faster than needed and agree with above just ignore angry people who dont want to help.
- Joined
- Oct 20, 2005
- Messages
- 16,911
- Reaction score
- 47,676
Sick and the venous pH was 7.2 (meaning an arterial would be almost 7.25)? That doesn't make a lot of sense.
Anyway, some of the hypokalemia is urine loss, some is acidemia. Given some infusion of Insulin and K+ and they'll be alright. 20 versus 40 mEq? Meh.
As for a CVL, I actually can't remember the last time I've seen a CVL placed for a DKA.
Anyway, some of the hypokalemia is urine loss, some is acidemia. Given some infusion of Insulin and K+ and they'll be alright. 20 versus 40 mEq? Meh.
As for a CVL, I actually can't remember the last time I've seen a CVL placed for a DKA.
I agree with all of the above, especially Turkeyjerkey had my thoughts exactly. Mag was normal so we didn't replace - is it still a thing to give IV mag even if its WNL? We gave 3L LR up front and would have done more if pt stayed with us longer. I also haven't needed to place a central line in DKA before. Thanks everyone for feedback - I appreciate it!
- Joined
- Oct 10, 2007
- Messages
- 4,253
- Reaction score
- 7,081
Generally need to check labs every 3-4 hours while on insulin gtt (or q1h ISS though I prefer gtt due to better predictability especially if any concurrent renal disease plus nursing requirement is essentially the same). It is uncommon but some of the older diabetics with trashed vascular systems that nobody can get decent IVs on (who always present in the middle of the night) ill drop a CVL so I dont get over 9000 phone calls about not being able to draw labs or catch up with K replacement of crying because the K hurts etc.I agree with all of the above, especially Turkeyjerkey had my thoughts exactly. Mag was normal so we didn't replace - is it still a thing to give IV mag even if its WNL? We gave 3L LR up front and would have done more if pt stayed with us longer. I also haven't needed to place a central line in DKA before. Thanks everyone for feedback - I appreciate it!
- Joined
- Apr 27, 2014
- Messages
- 863
- Reaction score
- 1,501
Did the person die?
Did they suffer permanent end organ damage?
Did they suffer an injury that will prolong los?
If the answer to those three questions is no, I am already yawning. Being a jerk is rarely needed, and should be saved for when it matters. If you prefer something happen differently or are worried it could lead to one of the things above at some point it makes sense to tell them.
To answer the question I would also probably have gone the po/iv route outlined above, and started insulin drip after first round, even if only at a low dose with a boatload of fluid, some of which would have k in it. But I doubt it matters
Did they suffer permanent end organ damage?
Did they suffer an injury that will prolong los?
If the answer to those three questions is no, I am already yawning. Being a jerk is rarely needed, and should be saved for when it matters. If you prefer something happen differently or are worried it could lead to one of the things above at some point it makes sense to tell them.
To answer the question I would also probably have gone the po/iv route outlined above, and started insulin drip after first round, even if only at a low dose with a boatload of fluid, some of which would have k in it. But I doubt it matters
- Joined
- Jun 9, 2016
- Messages
- 1,242
- Reaction score
- 2,209
Barring features not being shared, this is not a particularly sick DKA and there's no rush at all to get fancy with the potassium to expedite insulin. Give 2-4g of Mg. 10-20 meq/h k infusion as KCl or KPhos + 40 PO. Bolus a couple liters of LR and then run it at 150-200/hr. Recheck K at 4 hr. They're not profoundly acidemic, altered, etc. No insulin bolus. Start gtt @ 0.05ish once K>3.3ish and uptitrate your gtt to 0.1 as your K permits. Most of what constitutes good DKA care imo is avoiding harm
- Joined
- Apr 27, 2014
- Messages
- 863
- Reaction score
- 1,501
Barring features not being shared, this is not a particularly sick DKA and there's no rush at all to get fancy with the potassium to expedite insulin. Give 2-4g of Mg. 10-20 meq/h k infusion as KCl or KPhos + 40 PO. Bolus a couple liters of LR and then run it at 150-200/hr. Recheck K at 4 hr. They're not profoundly acidemic, altered, etc. No insulin bolus. Start gtt @ 0.05ish once K>3.3ish and uptitrate your gtt to 0.1 as your K permits. Most of what constitutes good DKA care imo is avoiding harm
starting insulin drips at 0.05units/hr seems unlikely to be adding much if it’s not following an initial bolus. If you’re going to do that I would just wait personally.
- Joined
- Jun 9, 2016
- Messages
- 1,242
- Reaction score
- 2,209
starting insulin drips at 0.05units/hr seems unlikely to be adding much if it’s not following an initial bolus. If you’re going to do that I would just wait personally.
Just to be sure since you spelled out the units, you know I mean 0.05 u/kg/h yes? I'd need to double check adults, but there's noninferiority data for 0.05 VS 0.1 in peds DKA and I care about lyte disturbances considerably more in adults. Start 0.05 and if tol ramp up to 0.1 to speed closure if desired. No role for bolus either way imo
- Joined
- Apr 27, 2014
- Messages
- 863
- Reaction score
- 1,501
Just to be sure since you spelled out the units, you know I mean 0.05 u/kg/h yes? I'd need to double check adults, but there's noninferiority data for 0.05 VS 0.1 in peds DKA and I care about lyte disturbances considerably more in adults. Start 0.05 and if tol ramp up to 0.1 to speed closure if desired. No role for bolus either way imo
That makes a lot more sense. Although im slightly disappointed, I wanted to learn more about homeopathic insulin.
Although I’m aware of standard dosing most places I worked have a home cooked protocol that empirically starts between 5-10 u/hr (which works out similarly) and then is titrated by nursing according to a protocol, requiring divine intervention to deviate from. I no longer consider dose in u/kg outside Peds very often.
- Joined
- Oct 5, 2015
- Messages
- 1,985
- Reaction score
- 1,916
Have seen a K of 1.4 and another 1.x K.
60 K po upfront followed by another 40 po K shortly afterwards. Done it many times with 0 issues. Give another 40 if able to tolerate (add zofran po unless qtc >500).
IV, who cares... as long as you get 20 going in total per hour. And 4g Mg upfront.
60 K po upfront followed by another 40 po K shortly afterwards. Done it many times with 0 issues. Give another 40 if able to tolerate (add zofran po unless qtc >500).
IV, who cares... as long as you get 20 going in total per hour. And 4g Mg upfront.
Don’t check it. Just give it (in this case).Stupid question but did you check the Mg?
- Joined
- Jun 17, 2012
- Messages
- 40
- Reaction score
- 19
Agree with everything so far, but also keep in mind that there is zero utility in rechecking a potassium 1 hour after ordering 40 PO and an IV with a rate of 10meq/hr.
Also, a CVC has absolutely zero role in DKA in 2021. The only time that it would come in handy is if you need more IV sites than you are able to get peripherally. Now that we all have ultrasounds there really shouldn't ever be a need for CVC strictly for ACCESS issues.
They have horrible flow rates, and if you need to give IV fluids a well placed 18G in the arm will outrun the large port or your CVC.
Also, a CVC has absolutely zero role in DKA in 2021. The only time that it would come in handy is if you need more IV sites than you are able to get peripherally. Now that we all have ultrasounds there really shouldn't ever be a need for CVC strictly for ACCESS issues.
They have horrible flow rates, and if you need to give IV fluids a well placed 18G in the arm will outrun the large port or your CVC.
- Joined
- Dec 2, 2008
- Messages
- 995
- Reaction score
- 810
FWIW, give 20 meq via CVL over 30-40 mins all the time immed post CPB (still in the OR) with insulin running and AAI or DDD. If I let the ICU nurses finish it it'll be day after tomorrow before the K is corrected.
- Joined
- Dec 28, 2010
- Messages
- 4,955
- Reaction score
- 5,991
Hey all, EM trainee here, had a sick patient in small community ED with DKA BS600s, bicarb 8, AG 28, pH 7.2 on VBG and vitals normal (sx for over a week, compensated fairly well). No big deal except K was 2.8. 2 large bore peripheral IVs, started peripheral K infusion at 10meq/hr and PO 40meq, talked to ED pharmacy who said we could go up to 20meq/hr divided by both IVs... we rechecked in an hour and K was still like 2.9. At this point we just called for transfer to bigger local hospital ICU that was staffed by hospitalist, who chewed me out for not replacing K faster thereby delaying the insulin gtt, and said I should double it to 20meq/hr in each IV, aka total 40meq/hr. It was too busy for us to place central line but he said it was fine peripherally for a critical patient, short term, monitored, etc. I've never heard this before and it seemed like too much to me. Tried to do some research and I don't see much on this out there. Thoughts?
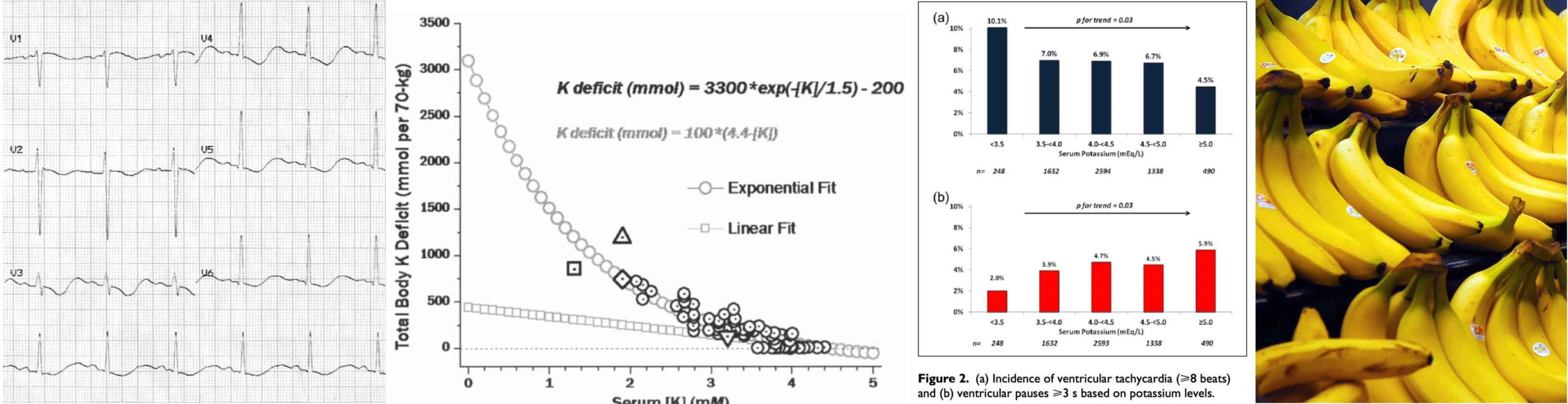
Insulin gtt should have been started right away to correct that anion gap IMO. If you didn't start it, that's probably what the quarterback/accepting hospitalist was upset about because the thing with Potassium in DKA is the acidosis draining it (H+ blood<-->K+ cell->K+ blood-> urine --> K+ deficit). Correcting that should be the first priority or else your repletion of K is akin to filling up a bathrub while the drain's open. Yes, I understand the insulin effect on serum K+ but it's already pretty low and I have a feeling that it wasn't a hyperacute thing that needed to fixed that moment and you could have just given oral K/Mg prophylactically concurrent to the insulin gtt which at the least would counteract the K+ drop from the insulin and then when the AG is corrected (i.e. K+ output drain is clogged) you could pump the K+ back in.
That's how I look at it.
Edit: Concur with the Mg+. Probably better to just replace it and check after unless it took up an extra line. A serum K+ of 2.8 in DKA is pretty low indicating maybe the patient had a Total Body K+ deficit they were living at for some time. Agree with LR too, would have made a small difference but its better for acidosis than NS and has neglible amounts of K. If the patient was getting NS as their MF, would have made sense to switch although sometimes pharmacists say stuff with LR clumping when mixed with other things (ceftiaxone off the top of my head).
Last edited:
- Joined
- Jun 9, 2016
- Messages
- 1,242
- Reaction score
- 2,209
Insulin gtt should have been started right away to correct that anion gap IMO. If you didn't start it, that's probably what the quarterback/accepting hospitalist was upset about because the thing with Potassium in DKA is the acidosis draining it (H+ blood<-->K+ cell->K+ blood-> urine --> K+ deficit). Correcting that should be the first priority or else your repletion of K is akin to filling up a bathrub while the drain's open. Yes, I understand the insulin effect on serum K+ but it's already pretty low and I have a feeling that it wasn't a hyperacute thing that needed to fixed that moment and you could have just given oral K/Mg prophylactically concurrent to the insulin gtt which at the least would counteract the K+ drop from the insulin and then when the AG is corrected (i.e. K+ output drain is clogged) you could pump the K+ back in.
That's how I look at it.
Edit: Concur with the Mg+. Probably better to just replace it and check after unless it took up an extra line. A serum K+ of 2.8 in DKA is pretty low indicating maybe the patient had a Total Body K+ deficit they were living at for some time. Agree with LR too, would have made a small difference but its better for acidosis than NS and has neglible amounts of K. If the patient was getting NS as their MF, would have made sense to switch although sometimes pharmacists say stuff with LR clumping when mixed with other things (ceftiaxone off the top of my head).
Disagree. The acidosis in DKA is generally reasonably well tolerated and 7.2 on a venous gas is a very modest acidosis for DKA. Like you're saying the K is serum shifted related to acidosis - when a DKA patient is hypokalemic they are profoundly whole body K deplete. Overly aggressive insulin without appropriate attention to K can lead to hypokalemic arrest, which I'm personally aware of one recent incidence of at one of my hospitals but fortunately with a good outcome. Sit on the insulin unless there's a really pressing indication and fix your K
- Joined
- Dec 28, 2010
- Messages
- 4,955
- Reaction score
- 5,991
Disagree. The acidosis in DKA is generally reasonably well tolerated and 7.2 on a venous gas is a very modest acidosis for DKA. Like you're saying the K is serum shifted related to acidosis - when a DKA patient is hypokalemic they are profoundly whole body K deplete. Overly aggressive insulin without appropriate attention to K can lead to hypokalemic arrest, which I'm personally aware of one recent incidence of at one of my hospitals but fortunately with a good outcome. Sit on the insulin unless there's a really pressing indication and fix your K
OK. Thanks for telling me this and good to know. If this issue comes up I’ll know what to do.
- Joined
- Sep 27, 2008
- Messages
- 3,015
- Reaction score
- 2,223
That was a bizarre bump and sequence of posts
- Joined
- Jan 18, 2014
- Messages
- 4,098
- Reaction score
- 4,063
max k of 20 meq/hr is fairly standard on a monitored bed - I wouldn't go faster than that unless absolutely necessary - in this case I would argue it wasn't. I would also not want to start the insulin drip until you saw a trend in the correct direction, if you felt the insulin drip couldn't wait - draw K q 1 hour (hopefully you have a POC machine vs waiting on lab) and immediately stop if K drops - like is stated, this pt is likely whole body deleted, and we all know low K can cause arrest.
I’ve seen patients get 40-50 meq/hr without issue as long as their access is appropriate.max k of 20 meq/hr is fairly standard on a monitored bed - I wouldn't go faster than that unless absolutely necessary - in this case I would argue it wasn't. I would also not want to start the insulin drip until you saw a trend in the correct direction, if you felt the insulin drip couldn't wait - draw K q 1 hour (hopefully you have a POC machine vs waiting on lab) and immediately stop if K drops - like is stated, this pt is likely whole body deleted, and we all know low K can cause arrest.
- Joined
- Jan 18, 2014
- Messages
- 4,098
- Reaction score
- 4,063
The cardiac consequences are not related to the type of access (the burning sensation is). It isn't an issue until, well it is - and the heart stops. Some places do allow 40 - my institution puts 20 as a max (major cardiac center)I’ve seen patients get 40-50 meq/hr without issue as long as their access is appropriate.
- Joined
- Dec 26, 2006
- Messages
- 7,100
- Reaction score
- 17,534
As an aside, in the OR I've given 20meq over 5-10 min so many times (through a good IV) that I've lost count. Of course, I'm standing right there watching the EKG and hemodynamics and I've got grams of calcium chloride at my disposal, but the reality is that the "danger" of infusing K too fast in someone with a normal rhythm and normal kidney function is wildly overblown.FWIW, give 20 meq via CVL over 30-40 mins all the time immed post CPB (still in the OR) with insulin running and AAI or DDD. If I let the ICU nurses finish it it'll be day after tomorrow before the K is corrected.
Your institution being a major cardiac center likely means they do a lot of cath and CABG. Does not really lend credence to this discussion. If someone’s K is 1.5 I’m not maxing out their repletion at 20 meq/hour….The cardiac consequences are not related to the type of access (the burning sensation is). It isn't an issue until, well it is - and the heart stops. Some places do allow 40 - my institution puts 20 as a max (major cardiac center)
I just realized you are a pharmacist. Sometimes the guidelines you folks are familiar with are in somewhat of vacuum. Much of being a physician is examining the whole situation and weighing risks/benefits/alternatives.
- Joined
- Jan 18, 2014
- Messages
- 4,098
- Reaction score
- 4,063
not sure if that was intended as a backhanded insult or not - but I am well aware that you don't just follow numbers in a vacuum - for what it is worth I asked on our board a similar question - and got a variety of answers, some of which had hospitals with ridiculous protocols (only intensivists can order more than 20 meq of KCL regardless of how low the k is and how long they replace over).I just realized you are a pharmacist. Sometimes the guidelines you folks are familiar with are in somewhat of vacuum. Much of being a physician is examining the whole situation and weighing risks/benefits/alternatives.
I will fully admit when I am wrong, or have misinformation - and always looking to learn - FWIW I staff 100% in the ED/ICU (I don't do distribution) and I have never seen a MD want K to be given faster than the 20 meq an hour.
Some people talked about giving it during a code with hypokalemia as a cause - I personally have never seen this (and for a reference point due to the nature of my position I attend more codes than any other individual in my hospital as I cover the entire hospital from a code perspective at night) - obviously just because I attend them doesn't mean I know everything - just pointing out my observations.
- Joined
- May 19, 2016
- Messages
- 422
- Reaction score
- 403
DKA appears easy on the surface but is incredibly complex. It's also very satisfying to get someone out of DKA relatively quickly. It's such a common illness so people think a protocol is all you need. But there needs to be a lot of oversight to do it right. As said above, I would give 40 PO x2 as tolerated. At the same time give 20meq/hr. This patient is definitely total body K deplete. They also need probably 2 L or so LR or plasmalyte. And also 2-4mg of Mg. I basically always avoid NS. I would give SubQ long acting insulin since it takes a bit of time for that to kick start. I don't think I would start insulin drip until the K is above 3.3. Checking lytes every 4 hours. But I don't know what the data is on just starting a drip without an IV bolus. Would be interested in that as one poster said above they do for peds apparently without issue. Since this patient does not appear "sick" I wouldn't be too quick on accidentally bringing down his K any lower with a quicker acting IV insulin.
I’ve reached my limit on how much effort I can put into this exchange.not sure if that was intended as a backhanded insult or not - but I am well aware that you don't just follow numbers in a vacuum - for what it is worth I asked on our board a similar question - and got a variety of answers, some of which had hospitals with ridiculous protocols (only intensivists can order more than 20 meq of KCL regardless of how low the k is and how long they replace over).
I will fully admit when I am wrong, or have misinformation - and always looking to learn - FWIW I staff 100% in the ED/ICU (I don't do distribution) and I have never seen a MD want K to be given faster than the 20 meq an hour.
Some people talked about giving it during a code with hypokalemia as a cause - I personally have never seen this (and for a reference point due to the nature of my position I attend more codes than any other individual in my hospital as I cover the entire hospital from a code perspective at night) - obviously just because I attend them doesn't mean I know everything - just pointing out my observations.
- Joined
- Dec 26, 2006
- Messages
- 7,100
- Reaction score
- 17,534
Despite your single center personal experience, limiting infusion to 20 meq/hr *regardless of the circumstances* is quite wrong.I will fully admit when I am wrong, or have misinformation - and always looking to learn - FWIW I staff 100% in the ED/ICU (I don't do distribution) and I have never seen a MD want K to be given faster than the 20 meq an hour.
- Joined
- Jan 18, 2014
- Messages
- 4,098
- Reaction score
- 4,063
I have more than “single center experience” never said regardless of the circumstances.Despite your single center personal experience, limiting infusion to 20 meq/hr *regardless of the circumstances* is quite wrong.
Last edited:
- Joined
- Dec 26, 2006
- Messages
- 7,100
- Reaction score
- 17,534
Ok. Just wanted to make sure that when you said that you've never seen an MD want more than 20 of K per hour that that wasn't some kind of implicit statement or recommendation that it should never be done, or that there was some strong evidence against doing it when the situation warrants it.I have more than “single center experience” never said regardless of the circumstances.
From Farkas's IBCC
Hypokalemia
CONTENTS Rapid Reference 🚀 Physiology: Potassium pharmacokinetics Diagnosis Clinical significance Causes Workup Risk stratification Treatment Target potassium level? Enteral route generally preferred Intravenous potassium Magnesium repletion Other measures Podcast Questions & discussion Pitfalls...
Medscape rx
- Joined
- Nov 1, 2007
- Messages
- 1,575
- Reaction score
- 1,169
DKA appears easy on the surface but is incredibly complex. It's also very satisfying to get someone out of DKA relatively quickly. It's such a common illness so people think a protocol is all you need. But there needs to be a lot of oversight to do it right. As said above, I would give 40 PO x2 as tolerated. At the same time give 20meq/hr. This patient is definitely total body K deplete. They also need probably 2 L or so LR or plasmalyte. And also 2-4mg of Mg. I basically always avoid NS. I would give SubQ long acting insulin since it takes a bit of time for that to kick start. I don't think I would start insulin drip until the K is above 3.3. Checking lytes every 4 hours. But I don't know what the data is on just starting a drip without an IV bolus. Would be interested in that as one poster said above they do for peds apparently without issue. Since this patient does not appear "sick" I wouldn't be too quick on accidentally bringing down his K any lower with a quicker acting IV insulin.
I don't think there is any utility (but there is a significant risk of harm) in giving a bolus of IV insulin for Type 1 Diabetics. As a PICU attending, the ER (usually due to poorly written triage protocols) giving bolus dose insulin grinds my gears. I don't need them to drop their sugar by more than 50 points in an hour. I do have a problem if they drop by 200. If it takes them 20 hours to get out of DKA instead of 14 or 16, who cares? The management of DKA is about avoiding cerebral edema and death, much more than it is about getting them out of DKA quickly. I'm ok with giving their home lantus dose at some point during the process, but our Endocrinologists have a lot of practice variation in regards to that, so we usually leave that decision to them.
In the type 2 diabetics, the bolus dose of IV insulin is less of a worry. Still not sure it's of any significant benefit, but not nearly so fraught as it is for the type 1s who are usually exquisitely sensitive to any available insulin.
as for potassium, we just use larger doses in our IV fluids (varies by center exact additives, but usually 30meq/L KCl and 30meq/L of Kphos or KAcetate) if K is less than 3.5. Still start the insulin drip. Personally if still low at 4 hour mark, may give additional bolus of 1meq/kg or 20meq (pharmacy limit).
Maybe in adults you need to be more worried about kidney injury related to the acidosis/hyperchloremia, but also don't think that the NS vs balanced fluids debate outside of patients in actual shock is enough to move the needle generally (genuinely curious what's the NNT for such concerns specifically in DKA without shock?), they are hypovolemic sure, but aren't subject to the ongoing high volume aggressive resuscitation that a patient with sepsis might be.
- Joined
- Feb 27, 2015
- Messages
- 2,265
- Reaction score
- 4,222
I don't think there is any utility (but there is a significant risk of harm) in giving a bolus of IV insulin for Type 1 Diabetics. As a PICU attending, the ER (usually due to poorly written triage protocols) giving bolus dose insulin grinds my gears. I don't need them to drop their sugar by more than 50 points in an hour. I do have a problem if they drop by 200. If it takes them 20 hours to get out of DKA instead of 14 or 16, who cares? The management of DKA is about avoiding cerebral edema and death, much more than it is about getting them out of DKA quickly. I'm ok with giving their home lantus dose at some point during the process, but our Endocrinologists have a lot of practice variation in regards to that, so we usually leave that decision to them.
In the type 2 diabetics, the bolus dose of IV insulin is less of a worry. Still not sure it's of any significant benefit, but not nearly so fraught as it is for the type 1s who are usually exquisitely sensitive to any available insulin.
as for potassium, we just use larger doses in our IV fluids (varies by center exact additives, but usually 30meq/L KCl and 30meq/L of Kphos or KAcetate) if K is less than 3.5. Still start the insulin drip. Personally if still low at 4 hour mark, may give additional bolus of 1meq/kg or 20meq (pharmacy limit).
Maybe in adults you need to be more worried about kidney injury related to the acidosis/hyperchloremia, but also don't think that the NS vs balanced fluids debate outside of patients in actual shock is enough to move the needle generally (genuinely curious what's the NNT for such concerns specifically in DKA without shock?), they are hypovolemic sure, but aren't subject to the ongoing high volume aggressive resuscitation that a patient with sepsis might be.
I know in adults, there's a well established NNH for adverse kidney events of around 100 when giving N/S over balanced solutions for all comers to the ED, both admitted to the ward or to the ICU as per the SALT-ED, SMART-SURG, and SMART-MED trials. I just don't give normal saline anymore unless there's a very good reason (severe metabolic alkalosis, Addisonian crisis, resuscitation when the nurses don't have time to look up compatibility, head injury and no Plasmalyte, etc.).
I've also had great success using the Umpierrez protocol for subcutaneous insulin and PO potassium in a resource limited setting. I think there's a lot of dogma around IV insulin in DKA.
https://pubmed.ncbi.nlm.nih.gov/15277410/
Last edited:
- Joined
- Jun 9, 2016
- Messages
- 1,242
- Reaction score
- 2,209
I know in adults, there's a well established NNH for adverse kidney events of around 100 when giving N/S over balanced solutions for all comers to the ED, both admitted to the ward or to the ICU as per the SALT-ED, SMART-SURG, and SMART-MED trials. I just don't give normal saline anymore unless there's a very good reason (severe metabolic alkalosis, Addisonian crisis, resuscitation when the nurses don't have time to look up compatibility, head injury and no Plasmalyte, etc.).
I've also had great success using the Umpierrez protocol for subcutaneous insulin and PO potassium in a resource limited setting. I think there's a lot of dogma around IV insulin in DKA.
https://pubmed.ncbi.nlm.nih.gov/15277410/
Agreed, I don't use NS unless there's a specific reason to use NS, with the exception of most kids under a given age (different thresholds for different people, somewhere between 1 and 2 probably) where I mostly avoid LR just due to possibility of undiagnosed inborn errors of metabolism, though in those cases my understanding is plasmalyte is likely fine. I particularly dislike NS in DKA because our agreement with our endocrinologists is to treat to a bicarb threshold (which makes no logical sense to me versus a gap threshold but regardless) and that becomes frustrating with hyoerchloremia. I have no reason to believe the physiology of hyperchloremia is significantly different in peds from adults, and I believe at least one paper recently (past 6 months-ish?) published substantiating AKI risk in a pediatric population though I'd have to look for it. I certainly don't think we're harming to any meaningful degree the relatively well patients with saline, but if there's not a reason specifically to use saline I just don't see why I would use it as a default. All that being said our DKA protocol uses saline.
- Joined
- Nov 1, 2007
- Messages
- 1,575
- Reaction score
- 1,169
Agreed, I don't use NS unless there's a specific reason to use NS, with the exception of most kids under a given age (different thresholds for different people, somewhere between 1 and 2 probably) where I mostly avoid LR just due to possibility of undiagnosed inborn errors of metabolism, though in those cases my understanding is plasmalyte is likely fine. I particularly dislike NS in DKA because our agreement with our endocrinologists is to treat to a bicarb threshold (which makes no logical sense to me versus a gap threshold but regardless) and that becomes frustrating with hyoerchloremia. I have no reason to believe the physiology of hyperchloremia is significantly different in peds from adults, and I believe at least one paper recently (past 6 months-ish?) published substantiating AKI risk in a pediatric population though I'd have to look for it. I certainly don't think we're harming to any meaningful degree the relatively well patients with saline, but if there's not a reason specifically to use saline I just don't see why I would use it as a default. All that being said our DKA protocol uses saline.
I would love to make the change to LR in my large multi campus children’s hospital system. For now just satisfied that we don’t see 1/4NS with any regularity anymore.
Agree that the endocrine fixation on bicarb levels is perpetually annoying.
