okay, i keep hearing the phrase 'status post' but i don't know what it means. can someone explain it? and how is it used?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
what is 'status post' and how to use it?
- Thread starter EPO
- Start date
- Joined
- Jul 26, 2000
- Messages
- 2,615
- Reaction score
- 16
status post is used to designate when someone has had a significant procedure/event happen.
if some guy comes in with chest pain, you want to know if he's had a coronary artery bypass graft, or has had a heart attack before. so you'd say something like:
this is a 55yo caucasian male status post MI in 1992, status post CABG x 2, etc.
you use it for procedures/events. another example would be someone who comes in with left sided facial droop and left sided weakness you'd be like:
this is a 72 yo female status post CVA in 2000 etc etc
any surgical procedures of relevance or strokes, heart attacks, things like that. hope this helps.
if some guy comes in with chest pain, you want to know if he's had a coronary artery bypass graft, or has had a heart attack before. so you'd say something like:
this is a 55yo caucasian male status post MI in 1992, status post CABG x 2, etc.
you use it for procedures/events. another example would be someone who comes in with left sided facial droop and left sided weakness you'd be like:
this is a 72 yo female status post CVA in 2000 etc etc
any surgical procedures of relevance or strokes, heart attacks, things like that. hope this helps.
- Joined
- Apr 13, 2003
- Messages
- 663
- Reaction score
- 3
It's a little confusing at first. I've never heard anyone use it outside of medicine, so don't feel bad for not knowing. Listen to the way the residents use it and you'll pick it up quickly.
- Joined
- Jul 25, 2001
- Messages
- 9,319
- Reaction score
- 125
It's just one more piece of medicalese that is entirely unnecessary and helps turn an incredibly simple statement into something that the layperson can't understand. Med-speak irritates me to the point of apoplexy. What really bugs me is when med folks start using these terms in "real life." (I was late to work secondary to car trouble! I'm three days status post surgery final exam!)
Other commonly used med words that bug the sh1t out of me:
-Punky. "Mr. Thompson is a little punky today." STFU with your "punky." WTF. I'll show you punky.
-Appreciate. "Did you appreciate the inguinal hernia?" No, I didn't appreciate it, I felt it.
-Head is normocephalic and atraumatic. NO SH1T, oh, you mean like 99% of all patients on a non-ED service? This is like reporting on every single patient: "Patient's feet are both attached and have ten toes each!"
-Patient is a poor historian. WTF does this mean? Don't be such a puss, just say "Patient is a dipsh1t" or "Patient is senile and can't put three words together" or "Patient recalls their medical history about as well as I recall my college calculus."
-Shotty lymphadenopathy. Used all the time by everybody. Ask three different attendings what they mean by "shotty" and observe the three different answers.
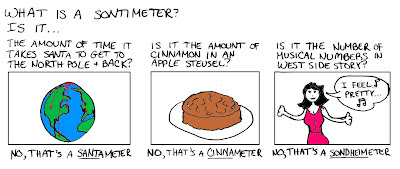
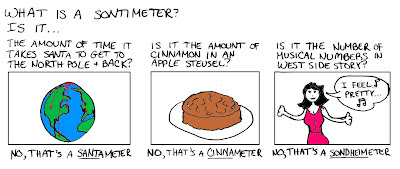
-Centimeter pronounced "sontimeter." F YOU. I swear to Christ I'm never going to change the way that I and everybody else in damn country pronounces "centimeter" just because it's some pretentious medical tradition.
I'm on surgery and I'm a little cranky.
Other commonly used med words that bug the sh1t out of me:
-Punky. "Mr. Thompson is a little punky today." STFU with your "punky." WTF. I'll show you punky.
-Appreciate. "Did you appreciate the inguinal hernia?" No, I didn't appreciate it, I felt it.
-Head is normocephalic and atraumatic. NO SH1T, oh, you mean like 99% of all patients on a non-ED service? This is like reporting on every single patient: "Patient's feet are both attached and have ten toes each!"
-Patient is a poor historian. WTF does this mean? Don't be such a puss, just say "Patient is a dipsh1t" or "Patient is senile and can't put three words together" or "Patient recalls their medical history about as well as I recall my college calculus."
-Shotty lymphadenopathy. Used all the time by everybody. Ask three different attendings what they mean by "shotty" and observe the three different answers.
-Centimeter pronounced "sontimeter." F YOU. I swear to Christ I'm never going to change the way that I and everybody else in damn country pronounces "centimeter" just because it's some pretentious medical tradition.
I'm on surgery and I'm a little cranky.
- Joined
- Apr 13, 2003
- Messages
- 663
- Reaction score
- 3
sacrament said:It's just one more piece of medicalese that is entirely unnecessary and helps turn an incredibly simple statement into something that the layperson can't understand. Med-speak irritates me to the point of apoplexy. What really bugs me is when med folks start using these terms in "real life." (I was late to work secondary to car trouble! I'm three days status post surgery final exam!)
The only time I've ever heard anyone do something like this, they were ridiculed and humiliated and never did it again.
What does this even mean? I've never heard anyone say it. Maybe it's a regional thing.-Punky. "Mr. Thompson is a little punky today." STFU with your "punky." WTF. I'll show you punky.
I don't have any problem with this one since the word is actually being used correctly.-Appreciate. "Did you appreciate the inguinal hernia?" No, I didn't appreciatei it, I felt it.
Outside of the ED, I've only seen this used in peds, where it's actually a relevent finding.-Head is normocephalic and atraumatic. NO SH1T, oh, you mean like 99% of all patients on a non-ED service? This is like reporting on every single patient: "Patient's feet are both attached and have ten toes each!"
The problem I have with this is that you (the history taker) are the historian, not the patient. The patient is the informant. Either way, though, it's very important to convey so that you can deflect the blame for a poor HPI.-Patient is a poor historian. WTF does this mean? Don't be such a puss, just say "Patient is a dipsh1t" or "Patient is senile and can't put three words together" or "Patient recalls their medical history about as well as I recall my college calculus."
Again, another one I've never heard. Maybe another regional thing.-Shotty lymphadenopathy. Used all the time by everybody. Ask three different attendings what they mean by "shotty" and observe the three different answers.
This one bugs me too. It's been around for a long time. Here's a 9 year old thread from a newsgroup discussing the same thing: http://websom.hut.fi/websom/sci.lang-new/html/2_avx14.html-Centimeter pronounced "sontimeter." F YOU. I swear to Christ I'm never going to change the way that I and everybody else in damn country pronounces "centimeter" just because it's some pretentious medical tradition.
- Joined
- Jan 26, 2003
- Messages
- 1,254
- Reaction score
- 3
sacrament said:I'm on surgery and I'm a little cranky.
Don't apologize--that was entertaining ... I am finishing a summer of chart-review research, so I hear you.

- Joined
- Apr 26, 2002
- Messages
- 3,617
- Reaction score
- 10
sacrament said:It's just one more piece of medicalese that is entirely unnecessary and helps turn an incredibly simple statement into something that the layperson can't understand. Med-speak irritates me to the point of apoplexy. What really bugs me is when med folks start using these terms in "real life." (I was late to work secondary to car trouble! I'm three days status post surgery final exam!)
Other commonly used med words that bug the sh1t out of me:
-Punky. "Mr. Thompson is a little punky today." STFU with your "punky." WTF. I'll show you punky.
-Appreciate. "Did you appreciate the inguinal hernia?" No, I didn't appreciatei it, I felt it.
-Head is normocephalic and atraumatic. NO SH1T, oh, you mean like 99% of all patients on a non-ED service? This is like reporting on every single patient: "Patient's feet are both attached and have ten toes each!"
-Patient is a poor historian. WTF does this mean? Don't be such a puss, just say "Patient is a dipsh1t" or "Patient is senile and can't put three words together" or "Patient recalls their medical history about as well as I recall my college calculus."
-Shotty lymphadenopathy. Used all the time by everybody. Ask three different attendings what they mean by "shotty" and observe the three different answers.
-Centimeter pronounced "sontimeter." F YOU. I swear to Christ I'm never going to change the way that I and everybody else in damn country pronounces "centimeter" just because it's some pretentious medical tradition.
I'm on surgery and I'm a little cranky.
I hate boggy edema 👎
- Joined
- Jul 25, 2001
- Messages
- 9,319
- Reaction score
- 125
I thought of another one today... using "times" for everything. "Patient had stool times three." WTF IS WRONG WITH SAYING "Patient had three BMs?" And why is "after" a p with a line over it instead of an a with a line over it, which inexplicably means "before?" (Yeah yeah, I know why, it's a rhetorical question, I'm just saying it's ridiculous to maintain useless and confusing traditions.)
- Joined
- May 16, 2001
- Messages
- 180
- Reaction score
- 0
I think some med-speak is actually derived from writing. Given that we have to write so much we tend to start using abbreviations and shorthand.
In reference to some of the examples already mentioned:
Patient had three bowel movements. = Pt had BM X3
Patient has a history of 2 cerebrovascular accidents. = Pt s/p CVA X2
BTW, thanks to the person who explained what a 'sontimeter' was, I'm in my 4th year of Med school and I still didn't know what that meant. I will NEVER use that word except to deride it. 😉
In reference to some of the examples already mentioned:
Patient had three bowel movements. = Pt had BM X3
Patient has a history of 2 cerebrovascular accidents. = Pt s/p CVA X2
BTW, thanks to the person who explained what a 'sontimeter' was, I'm in my 4th year of Med school and I still didn't know what that meant. I will NEVER use that word except to deride it. 😉
- Joined
- Aug 5, 2004
- Messages
- 506
- Reaction score
- 1
sacrament said:-Punky. "Mr. Thompson is a little punky today." STFU with your "punky." WTF. I'll show you punky.
What does this mean? I've never heard that.
- Joined
- Jul 25, 2001
- Messages
- 9,319
- Reaction score
- 125
fourthyearmed said:What does this mean? I've never heard that.
Maybe this is regional, because everybody and their brother uses it here. Basically, while some people have a personal specific meaning when they use it, in general it means "to look sick" or to look septic.
Smurfette
Gargamel always had a thing for blondes.
Staff member
Administrator
Volunteer Staff
20+ Year Member
- Joined
- Jun 7, 2001
- Messages
- 5,045
- Reaction score
- 4,602
sacrament said:-Punky. "Mr. Thompson is a little punky today." STFU with your "punky." WTF. I'll show you punky.
-Appreciate. "Did you appreciate the inguinal hernia?" No, I didn't appreciate it, I felt it.
-Head is normocephalic and atraumatic. NO SH1T, oh, you mean like 99% of all patients on a non-ED service? This is like reporting on every single patient: "Patient's feet are both attached and have ten toes each!"
-Patient is a poor historian. WTF does this mean? Don't be such a puss, just say "Patient is a dipsh1t" or "Patient is senile and can't put three words together" or "Patient recalls their medical history about as well as I recall my college calculus."
-Shotty lymphadenopathy. Used all the time by everybody. Ask three different attendings what they mean by "shotty" and observe the three different answers.
-Centimeter pronounced "sontimeter." F YOU. I swear to Christ I'm never going to change the way that I and everybody else in damn country pronounces "centimeter" just because it's some pretentious medical tradition.
LOL!


 I am so glad I'm not the only one who finds these phrases annoying.
I am so glad I'm not the only one who finds these phrases annoying.I've never heard "punky" before. Interesting.
Other phrases that drive me crazy:
1. Stooling. As in, "Is Mrs. X stooling?". Well, I don't know if she is at the moment, do you want me to ask? Whatever happened to "Has Mrs. X had a bowel movement yet?"
2. Emesis. Call it vomit, puke, whatever. To me, emesis is one of those words like "micturation", "lacrimation" or "mastication" that try to make the speaker sound intelligent but really make them sound pretentious. I don't mind using the term emesis as a noun when trying to describe the vomit("emesis has a bilious appearance") but when it's used like ("pt is currently having some emesis" or "pt had two episodes of emesis") I find it really annoying.
3. Disposition. TO me, disposition means personality/mood. Ms. X's disposition is pretty cheerful today. What do you mean when are we going to dispose of her? Is she coding or something? I just think the term as we use it has a horrible connotation to it.
4. urimeter. Please call it a foley or foley bag like the rest of us and don't sound so pompous.
5. "well-developed, well-nourished". Everyone knows this is code for "pt is fat". SO why not say "55 yo obese female" instead? I would argue that the patient is neither well-developed nor well-nourished as they likely are not eating a balanced diet and are eating high-fat, high calorie meals and are in less than top physical form.
- Joined
- Jul 25, 2001
- Messages
- 9,319
- Reaction score
- 125
sacrament said:(Yeah yeah, I know why, it's a rhetorical question,
Mumpu said:Overscored a and p are from Latin, like most other abbreviations.
And yet I knew, I knew, somebody would tell me anyway.
- Joined
- Jul 19, 2003
- Messages
- 94
- Reaction score
- 1
Speaking of medicalese...
Here's a good one...i saw this on an ER chart yesterday. See if you guys can interpret this statement:
95 yo LOL NHR BIBA for FFT, cp, n/v, with BRBPR. Patient is s/p NSTEMI x 2 in 96 and 97 w/ 4V CABG in 03 c/b wound infxn, and c/o CP x 3 hrs. Patient ambulates with FWW, is s/p b/l THR and fell yesterday 2/2 to SE and LOC.
Here's a good one...i saw this on an ER chart yesterday. See if you guys can interpret this statement:
95 yo LOL NHR BIBA for FFT, cp, n/v, with BRBPR. Patient is s/p NSTEMI x 2 in 96 and 97 w/ 4V CABG in 03 c/b wound infxn, and c/o CP x 3 hrs. Patient ambulates with FWW, is s/p b/l THR and fell yesterday 2/2 to SE and LOC.
- Joined
- Jul 25, 2003
- Messages
- 1,614
- Reaction score
- 6
95 year old little old lady, nursing home resident, brought in by ambulance for FFT (even this one gets me), chest pain, nausea and vomiting, with bright red blood per rectum. Patient is status post Non-ST Elevation MI x 2 in 96 and 97 w/ 4 Vessel Coronary Artery Bypass Graft in 03 complicated by wound infxn, and complains of Chest pain x 3 hrs. Patient ambulates with Four Wheel Walker(I think), is status post bilateral Total Hip Replacement and fell yesterday 2/2 to SE(?) and Loss of consciousness.
- Joined
- Apr 13, 2003
- Messages
- 663
- Reaction score
- 3
Seaglass said:95 year old little old lady, nursing home resident, brought in by ambulance for FFT (even this one gets me), chest pain, nausea and vomiting, with bright red blood per rectum. Patient is status post Non-ST Elevation MI x 2 in 96 and 97 w/ 4 Vessel Coronary Artery Bypass Graft in 03 complicated by wound infxn, and complains of Chest pain x 3 hrs. Patient ambulates with Four Wheel Walker(I think), is status post bilateral Total Hip Replacement and fell yesterday 2/2 to SE(?) and Loss of consciousness.
FFT: never heard of it either (?falling from t___)
FFW: front-wheeled walker
SE: syncopal episode
The original is a horrible note. Of all notes, the ER note should be the easiest to decipher.
- Joined
- Jul 19, 2003
- Messages
- 94
- Reaction score
- 1
Jaded Soul said:FFT: never heard of it either (?falling from t___)
FFW: front-wheeled walker
SE: syncopal episode
The original is a horrible note. Of all notes, the ER note should be the easiest to decipher.
wow not bad! I guess all doctors can communicate no matter where they are or from in the country! sorry FFT was supposed to be FTT (Failure to Thrive).
2/2 = secondary
as for the note,...not only was it cryptic...it was illegible. I could only figure it out because i've seen those abrreviations a million times.
- Joined
- Apr 13, 2003
- Messages
- 663
- Reaction score
- 3
bariume said:wow not bad! I guess all doctors can communicate no matter where they are or from in the country! sorry FFT was supposed to be FTT (Failure to Thrive).
2/2 = secondary
as for the note,...not only was it cryptic...it was illegible. I could only figure it out because i've seen those abrreviations a million times.
Ah... I thought it might have been FTT, but usually applies to peds.
2/2 for "secondary to" is actually one of my favorites to use.
Not to revive an old thread but I just got into a "debate" with one of the attending concerning s/p. She said that we should just say "had" and that there was no difference. My response was that my understanding of "status post" is that the patient had the procedure performed and is proceeding as expected (without any complications). So for example..
25 yo male s/p appendectomy po (post op) day 3 states that the patient is in some mild pain/discomfort, has a surgical wound which is grossly doing well, no fevers, tolerating po intake, passing gas, peeing, not septic etc etc whatever else is expected of a patient on their 3rd day after the operation. I remember I hated this starting but once you actually start having to admit and write up 8-10 patients a day it's a real time saver.
and then it got ugly because my old teaching surgical attending walked by overheard and had at it with the other attnd...
Also concerning appreciate, it more or less implies that you were impressed for a hernia rather then just felt it because what you felt could very well not be a hernia.
NCAT very important for pediatric patients especially the younger ones (NC probably more important).
I figure most people use these abbreviations solely for the purpose of saving time, best example is G2P3003 as opposed to she had 2 pregnancies with 2 full term twins and 1 full term child all alive with no abortion and no premature births - all of which any OB/GYN attending would want to know.
BTW LOL - little old lady - LOL! but i doubt this is an approved abbreviation at any hospital.
And super late but doc05 don't be a douche
25 yo male s/p appendectomy po (post op) day 3 states that the patient is in some mild pain/discomfort, has a surgical wound which is grossly doing well, no fevers, tolerating po intake, passing gas, peeing, not septic etc etc whatever else is expected of a patient on their 3rd day after the operation. I remember I hated this starting but once you actually start having to admit and write up 8-10 patients a day it's a real time saver.
and then it got ugly because my old teaching surgical attending walked by overheard and had at it with the other attnd...
Also concerning appreciate, it more or less implies that you were impressed for a hernia rather then just felt it because what you felt could very well not be a hernia.
NCAT very important for pediatric patients especially the younger ones (NC probably more important).
I figure most people use these abbreviations solely for the purpose of saving time, best example is G2P3003 as opposed to she had 2 pregnancies with 2 full term twins and 1 full term child all alive with no abortion and no premature births - all of which any OB/GYN attending would want to know.
BTW LOL - little old lady - LOL! but i doubt this is an approved abbreviation at any hospital.
And super late but doc05 don't be a douche
- Joined
- Oct 10, 2011
- Messages
- 8,916
- Reaction score
- 11,383
LOL is one I've never seen.
Also, the importance of s/p is usually for things in the patient's medical history (at least from my experience)
For example, if you say patient had a STEMI 3 years ago without putting s/p CABGx4 vessels, your idea of what that person has (in terms of seriousness of disease and precipitating factors) is significantly different.
For patients that are days out of surgery, I usually just write, "Patient post-op day x, feeling better, had 1 BM last night, defer to surgery on d/c.
However, the BEST part of this is a note I saw one of my first weeks in.
"Continue ABx currently. Ask primary team to d/c on d/c"
Had no idea what it meant then, but now it all seems to simple.
Also, the importance of s/p is usually for things in the patient's medical history (at least from my experience)
For example, if you say patient had a STEMI 3 years ago without putting s/p CABGx4 vessels, your idea of what that person has (in terms of seriousness of disease and precipitating factors) is significantly different.
For patients that are days out of surgery, I usually just write, "Patient post-op day x, feeling better, had 1 BM last night, defer to surgery on d/c.
However, the BEST part of this is a note I saw one of my first weeks in.
"Continue ABx currently. Ask primary team to d/c on d/c"
Had no idea what it meant then, but now it all seems to simple.
- Joined
- Apr 18, 2012
- Messages
- 577
- Reaction score
- 698
"Continue ABx currently. Ask primary team to d/c on d/c"
Had no idea what it meant then, but now it all seems to simple.
Yeah, I still feel uncomfortable using d/c to mean both discontinue and discharge within the same note. I usually just use it to mean discontinue and write out discharge.
Also whoever said "sontimeters", that one is annoying as all hell. Someone used it today to say an "ET tube was 2 sontimeters too inferior". Here's my feeling about that: http://www.youtube.com/watch?v=9nz9-NWdsis&t=0m2s
- Joined
- Jul 8, 2008
- Messages
- 1,483
- Reaction score
- 7
I personally can't stand a lot of the back-formations in medspeak. One common kind makes a noun into a verb, eg when a pt has "anaphylaxis," you say they "anaphylaxed." Hideous as these are, I occasionally use them myself to save verbiage.
But there's another kind I really can't stand: fake singular forms of Latin plurals. For example, when people hear the plural form "varices" they assume the singular is "varice." It's "varix," goddamit! Same goes for radix (not radice) and naris (not nare). The worst of all is when someone hears a word that is already plural ending with -a, like "foramina," thinks it is singular and tries to "make" it plural by tacking on -e, eg "foraminae."
Yes, I have studied Latin in the past so this bothers me more than most people. But I'm not objecting to doctors not knowing Latin, but to the fact that they are just making **** up, and trying to sound learned when they have no idea what they're talking about.
If you don't know a word, you can always a) look it up or b) use a different word. But this made-up crap is so entrenched that most people don't even recognize the correct forms when they hear them, and some will even tell you they are "wrong."
But there's another kind I really can't stand: fake singular forms of Latin plurals. For example, when people hear the plural form "varices" they assume the singular is "varice." It's "varix," goddamit! Same goes for radix (not radice) and naris (not nare). The worst of all is when someone hears a word that is already plural ending with -a, like "foramina," thinks it is singular and tries to "make" it plural by tacking on -e, eg "foraminae."
Yes, I have studied Latin in the past so this bothers me more than most people. But I'm not objecting to doctors not knowing Latin, but to the fact that they are just making **** up, and trying to sound learned when they have no idea what they're talking about.
If you don't know a word, you can always a) look it up or b) use a different word. But this made-up crap is so entrenched that most people don't even recognize the correct forms when they hear them, and some will even tell you they are "wrong."
4
45408
No, it really doesn't imply that everything is "proceeding as expected." It just means that they had it done.Not to revive an old thread but I just got into a "debate" with one of the attending concerning s/p. She said that we should just say "had" and that there was no difference. My response was that my understanding of "status post" is that the patient had the procedure performed and is proceeding as expected (without any complications). So for example..
25 yo male s/p appendectomy po (post op) day 3 states that the patient is in some mild pain/discomfort, has a surgical wound which is grossly doing well, no fevers, tolerating po intake, passing gas, peeing, not septic etc etc whatever else is expected of a patient on their 3rd day after the operation. I remember I hated this starting but once you actually start having to admit and write up 8-10 patients a day it's a real time saver.
I don't really use it in conversation, but I use it in some dictations, and I use it a lot in handwritten notes. I'll use it as "POD 3 s/p sigmoid resection" in a progress note, or in a PMH, to indicate that yes, they have CAD, but it's now been treated, hence CAD s/p 3v CABG. Just please don't be redundant with it. I hate reading:
PMH:
1. History of diabetes (he still has it, so why is it a historical event?)
2. History of hypertension (still has that too)
3. History of obesity (and that)
4. Status post appendectomy.
5. Status post cholecystectomy.
6. Status post prostatectomy.
7. Status post ventral hernia repair.
If they have that many operations that you want to list, do it under a past surgical history.
I think we can let it go.And super late but doc05 don't be a douche
- Joined
- Feb 7, 2014
- Messages
- 1
- Reaction score
- 0
Overscored a and p are from Latin: anterior and posterior, with the meaning of before and after.
Smurfette
Gargamel always had a thing for blondes.
Staff member
Administrator
Volunteer Staff
20+ Year Member
- Joined
- Jun 7, 2001
- Messages
- 5,045
- Reaction score
- 4,602
in the us, overscored p usually means pending (a result)
Maybe it's a florida thing? I've seen P with a circle around it mean pending, pretty ubiquitously. I'm in the US and I've never personally seen p with an overscore mean anything other than "after" as Mendo described.
- Joined
- May 5, 2011
- Messages
- 133
- Reaction score
- 57
EPO is an SDN member of undetermined age and disposition now s/p explanation of "status post"
- Joined
- Feb 6, 2014
- Messages
- 686
- Reaction score
- 497
It's just one more piece of medicalese that is entirely unnecessary and helps turn an incredibly simple statement into something that the layperson can't understand.
Truth.
I work in FL, but lived in NY most of my life, so it might be an east coast thing. I've never heard of it being used as after before.Maybe it's a florida thing? I've seen P with a circle around it mean pending, pretty ubiquitously. I'm in the US and I've never personally seen p with an overscore mean anything other than "after" as Mendo described.
- Joined
- May 24, 2009
- Messages
- 4,672
- Reaction score
- 10,514
in the us, overscored p usually means pending (a result)
Definitely not where I live/practice (in the US . . . med school in the east, residency in the west). P with a circle around it is "pending", p with an overscore means "after/post".
Last edited:
- Joined
- Apr 9, 2000
- Messages
- 39,952
- Reaction score
- 18,721
Hmmm....east coast, west coast, international - I've worked in all of 'em and I've never seen p with an overscore mean anything but "post".
- Joined
- Dec 9, 2004
- Messages
- 4,514
- Reaction score
- 2,842
LOL!

I am so glad I'm not the only one who finds these phrases annoying.
5. "well-developed, well-nourished". Everyone knows this is code for "pt is fat". SO why not say "55 yo obese female" instead? I would argue that the patient is neither well-developed nor well-nourished as they likely are not eating a balanced diet and are eating high-fat, high calorie meals and are in less than top physical form.
I've never used WD/WN this way, nor is it what I assume to be the case when I read it. To me, it just means the patient isn't a dwarf (literally) or missing a limb and is neither obese nor cachectic. Maybe I'm the only one?
- Joined
- Jun 19, 2014
- Messages
- 1
- Reaction score
- 1
It's just one more piece of medicalese that is entirely unnecessary and helps turn an incredibly simple statement into something that the layperson can't understand. Med-speak irritates me to the point of apoplexy. What really bugs me is when med folks start using these terms in "real life." (I was late to work secondary to car trouble! I'm three days status post surgery final exam!)
-Centimeter pronounced "sontimeter." F YOU. I swear to Christ I'm never going to change the way that I and everybody else in damn country pronounces "centimeter" just because it's some pretentious medical tradition.
I'm on surgery and I'm a little cranky.
Reviving that old 2004 thread again, specifically to throw in my two cents on "sontimeter". Had multiple professors who pronounced centimeter as "sontimeter". So glad to see it's annoying and perceived as pretentious by a large majority of clinicians.
- Joined
- Dec 6, 2014
- Messages
- 3
- Reaction score
- 0
Huge like! Beautifully said! 🙂It's just one more piece of medicalese that is entirely unnecessary and helps turn an incredibly simple statement into something that the layperson can't understand. Med-speak irritates me to the point of apoplexy. What really bugs me is when med folks start using these terms in "real life." (I was late to work secondary to car trouble! I'm three days status post surgery final exam!)
Other commonly used med words that bug the sh1t out of me:
-Punky. "Mr. Thompson is a little punky today." STFU with your "punky." WTF. I'll show you punky.
-Appreciate. "Did you appreciate the inguinal hernia?" No, I didn't appreciate it, I felt it.
-Head is normocephalic and atraumatic. NO SH1T, oh, you mean like 99% of all patients on a non-ED service? This is like reporting on every single patient: "Patient's feet are both attached and have ten toes each!"
-Patient is a poor historian. WTF does this mean? Don't be such a puss, just say "Patient is a dipsh1t" or "Patient is senile and can't put three words together" or "Patient recalls their medical history about as well as I recall my college calculus."
-Shotty lymphadenopathy. Used all the time by everybody. Ask three different attendings what they mean by "shotty" and observe the three different answers.
-Centimeter pronounced "sontimeter." F YOU. I swear to Christ I'm never going to change the way that I and everybody else in damn country pronounces "centimeter" just because it's some pretentious medical tradition.
I'm on surgery and I'm a little cranky.
I thought a sontimeter was the distance that Sonta Claus travels in a minute.Reviving that old 2004 thread again, specifically to throw in my two cents on "sontimeter". Had multiple professors who pronounced centimeter as "sontimeter". So glad to see it's annoying and perceived as pretentious by a large majority of clinicians.
- Joined
- Apr 4, 2009
- Messages
- 17,237
- Reaction score
- 13,032
okay, i keep hearing the phrase 'status post' but i don't know what it means. can someone explain it? and how is it used?

- Joined
- Apr 26, 2006
- Messages
- 264
- Reaction score
- 85
Hmmm....east coast, west coast, international - I've worked in all of 'em and I've never seen p with an overscore mean anything but "post".
This. The only way I've seen "pending" abbreviated is a "p" with a circle around it.
An overscored p means "after".
Similar threads
- Replies
- 20
- Views
- 2K
D
- Replies
- 8
- Views
- 3K
