- Joined
- Dec 19, 2010
- Messages
- 10,255
- Reaction score
- 13,584
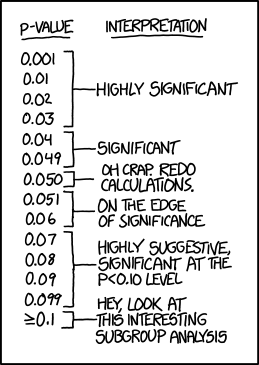
You're so confident in these guidelines, and the ones writing them are so confident in their absolute correctness, that they feel the need to "hedge," as you admit they "hedge"? If you're own concrete and unbendable guidelines are hedging, which side of the hedge are you on, on which day?What are you going for here? If you don't practice EBM *every*single*time*, you're a hypocrite for doing it at all? Sometimes there's gray areas, sometimes it's easier to do the wrong thing and it's pretty much without harm. It doesn't mean we should stop trying to do the right thing.
Which textbook are you referring to? Rosen's says antibiotics shouldn't be routinely used in strep throat (and following that textbook gives you added protection against Dr. Rosen should he target you to pad his bank account as a prosecuting expert witness). Looking over other professional organization websites, I'm not seeing any of them that say you should absolutely treat strep throat. They're all hedging, at the very least, and it looks like the pediatricians and family practice societies acknowledge that there's probably not much benefit to treating with antibiotics, even if their official policy still advocates testing and treatment.
I don't get railing against EBM. Sure, some errors are made, and I'm cool with people acknowledging that while what they're doing isn't in line with the latest EBM, they're going to do it anyway, because they're not comfortable changing their practice until more data becomes available. But using it like it's a bad word is the mindset that has the population pushing for laws to teach creationism instead of evolution in schools and failing to immunize their children.
I'm not saying that you should abandon the scientific method, for Pete's sake, but have some common sense in your practice and realize Medicine isn't, never was, and never will be, an exact science like Math. There is, was, and always will be that Art of Medicine. I will say, that does bother some people.
If you have trouble seeing this, just review Medical history and how much guidelines change year to year, decade to decade, and how studies done to answer the identical clinical questions often routinely contradict each other.
Steroids in spinal cord injury; they help, but they don't...tPA is good, but no, it's bad...Lipitor reduces cholesterol, so it must prevent heart attacks and death in people who haven't yet had them, but "oops," it doesn't, but not before it became the #1 selling drug on a planet of 7 billion people..Opiates were addictive, then they weren't anymore, now they are again.....I could go on for pages.
EBM is valuable. It's certainly better than blindly following dogma or asking a Witch Doctor what to do. But it's track record (and drug companies have a lot do with this, as do poor research technique, interpret and application) is actually exceedingly embarrassing if you step back and review it as a whole. It don't think the baby should be thrown out with the bath water, but I think this needs to be kept in mind.
If you stick around long enough, you'll see "unquestionable truth" in Medicine turn out to be false, then end up "true" again. Don't lose faith, just stay skeptical, and keep the latest and greatest at an arm's length.
Last edited: