- Joined
- Dec 12, 2003
- Messages
- 1,467
- Reaction score
- 948
So, it has been a while since we last had a clinical case for discussion. As usual, residents and fellows treat this as practice for oral boards (i.e. Say your rational for what you would like to do).
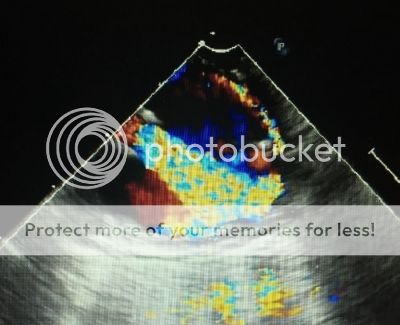
84 y/o male with Past Med Hx significant for hypertension sees his PCM for progressive dyspnea over the past 1-2 years and new development of exertional angina. PCM does a cardiac exam and hears a loud systolic murmur and sends the patient for TTE. Echo reveals EF 35-40% with severe calcific AS (Valve Area 0.48 cm2), mod AI, and inferior wall hypokinesis. Pt was then sent for Cath that showed two vessel disease. Admitted for further workup and found to have Creatnine 1.6. Also found to have asymptomatic 90%+ right sided Carotid stenosis on U/S, confirmed by CT Angiography. CTA head shows patent Circle of Willis. Pt denies any pulmonary, endocrine, GI, or neurologic issues. Surgeon schedules patient for CEA/AVR/CABG in same procedure. Surgeon notes that he would prefer that the Carotid be done prior to the cardiac procedure.
Lets start with Preoperative Concerns and then move to how you want manage this patient Perioperatively
84 y/o male with Past Med Hx significant for hypertension sees his PCM for progressive dyspnea over the past 1-2 years and new development of exertional angina. PCM does a cardiac exam and hears a loud systolic murmur and sends the patient for TTE. Echo reveals EF 35-40% with severe calcific AS (Valve Area 0.48 cm2), mod AI, and inferior wall hypokinesis. Pt was then sent for Cath that showed two vessel disease. Admitted for further workup and found to have Creatnine 1.6. Also found to have asymptomatic 90%+ right sided Carotid stenosis on U/S, confirmed by CT Angiography. CTA head shows patent Circle of Willis. Pt denies any pulmonary, endocrine, GI, or neurologic issues. Surgeon schedules patient for CEA/AVR/CABG in same procedure. Surgeon notes that he would prefer that the Carotid be done prior to the cardiac procedure.
Lets start with Preoperative Concerns and then move to how you want manage this patient Perioperatively