- Joined
- Sep 7, 2014
- Messages
- 3,220
- Reaction score
- 5,951
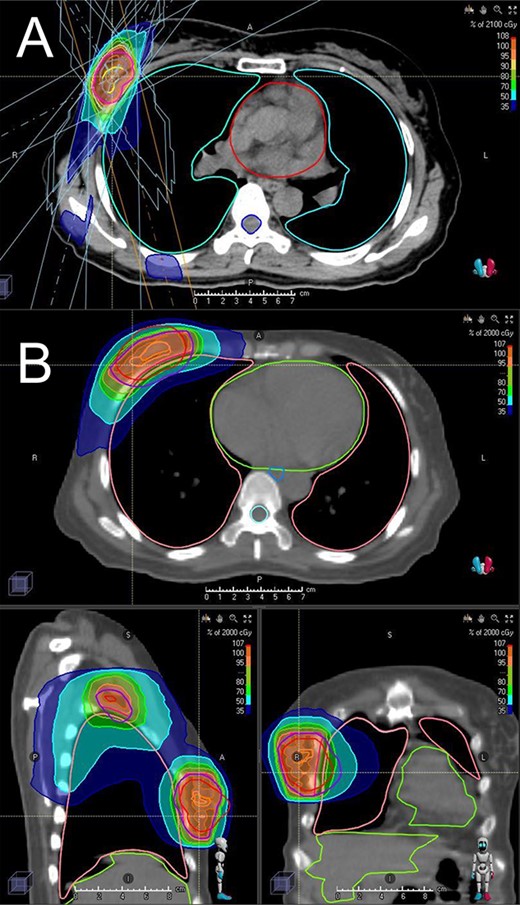
Well the nice thing about VMAT PBI is you can actually dose escalate while not changing the prescription dose. The dirty secret we never really talk about are the absurd coverage constraints in breast, even on trial. I think the IMN constraint that's acceptable is like 80-90% to 90%. I imagine when these trials are designed, investigators are saying, "meh, it's breast." VMAT PBI would allow you to actually cover the whole volume with 98%+ of the script. You could try this with 3D as well of course, just seems easier to pull off with VMAT without massive hotspots.I get that. But among the rationale for smaller treatment volumes in other disease sites is the corresponding ability to dose escalate for improved local control.
We have all this boost data that impacts local control. I'm not a big booster fwiw.
Is a (potentially) softer lumpectomy bed worth a 0.5% to 2% difference in recurrence?
I don't know.