- Joined
- Feb 13, 2012
- Messages
- 1,693
- Reaction score
- 1,946
Just going in order, sorry.
You good.Just going in order, sorry.
Do you know practicing surgeons who have herniated lumbar discs? In your opinion, would someone with an asymptomatic herniated disc be fit for surgical specialties, specifically neurosurgery?
Weird... I was just thinking about this the other day.Are there many surgeons who have stopped playing sports to prevent injuries that would impede them from performing surgeries? What would happen if a surgeon did injure like his finger or hand?
Are you required to be up to date on neurological studies? It seems like its a field (neuroscience) that is always coming up with something new. Are you held to some sort of monthly seminar requirement or is it just something you are expected to know during your freetime.
No, I have not seen a functional/ pain surgeon. Mine is nothing near what was in that video. Mine is cervical, i.e. it's in my neck and shoulders. I get "un-voluntary" spasms and contortions of my posterior neck muscles. They are called un-voluntary b/c I can keep from contorting and twisting, but the urge gets so incredibly overwhelming that I have to. My neurologist sucks. She's only good for botox, which helps a little, but very little. Doctors don't know exactly what causes it. I think the only surgical treatment is one when they do some kind of denervation, essentially kill (for a while) the nerves that have the most action with the pretense of lessening the dystonic "storms."
They also have some kind of deep brain stimulation where they drill a teeny hole in your cranium and install some wires somewhere on your brain. No thank you there. I'm tired of taking Xanax and Klonpin for the spasms, and the botox works less and less every time (sigh). My primary provider just referred me out to a pain management specialist. Of course, I'm not asking for medical advice here because that is not what this forum is for.
It wasn't factor XII Deficiency. I have antiphospholipid antibodies in my attacking my platelets. The hematologist said it's like APS, without the actual syndrome. So, the prolonged PTT was actually paradoxical, like a false positive. I actually clot more then I'm supposed to. For now, I do nothing, not even a low-dose aspirin, and I'm cleared for surgery.
Hi @neusu. A few months ago I let you know that I succeeded to find a shadowing position with a NS who does minimally invasive spine work. Just wanted to say that the smell of burning flesh and bone was not as bad as I was expecting.
The lifestyle in NS just seems so continuous and intense!
Do you know practicing surgeons who have herniated lumbar discs? In your opinion, would someone with an asymptomatic herniated disc be fit for surgical specialties, specifically neurosurgery?
Are there many surgeons who have stopped playing sports to prevent injuries that would impede them from performing surgeries? What would happen if a surgeon did injure like his finger or hand?
So, from your experience, how did you take everything (emotionally-wise) with all the added pressure. I do have anxiety; however, I was just wondering how you coped with that.
Hi @neusu, you are amazing for answering these questions. It took me about 3 days to go from page 1 to 19, but you have helped so many people out (including answering various repeated questions with patience and politeness).
Here's my question:
How well do you think homosexuals are accepted in neurosurgery in these days by their co-residents, fellows, and attendings? I'm sure this will change as millenials fill residency positions, but I think the change will be rather conservative.
Do you think non-effeminate homosexual males will generally be more accepted than a more effeminate one? On this note, do you know any homosexual males or females in neurosurgery?
Is there a factor of machismo involved in work (like, say, a stereotypical surgeon or ortho) no matter whether male/female?

Thanks for responding!Everyone adapts to residency differently and in their own way. I personally, tend to be outwardly smooth so people often can not really tell if I am anxious, nervous, or internally flailing. I think this may have helped, in some regard, because as the situation around me devolves I can maintain a presence of control and authority, despite often wanting to join the fray of knee-jerk reactions and escalation.
Residency, and life in general as a resident, is very emotionally taxing. Having balance and the ability to decompress is important. Having hobbies, activities, and a life outside the hospital is important, but maintaining relationships or activities that are enjoyable takes compromise. I may enjoy running, but spending an hour every day and a couple hours on the weekend simply is not very realistic. Adjusting my perspective and goals has helped. I still find time to do the things I enjoy, just it doesn't define me in the way it did formerly.
It is natural to have anxiety. Playing the guessing game and focusing on "what-ifs," however, can make this problematic. Learning how to address anxiety, be direct, and address things that create anxiety helps to overcome.
Neusu, perfect timing. My old PI is a neurosurgeon at a school hospital, and while I worked for him he taught myself and a friend to magnetically adjust cerebrospinal shunt valves, as well as the initial cranial nerve tests. After a few months he let us do it for him among other things, and he would supervise at all times. Is it alright for me to mention this on the amcas, I thought it was cool, but I don't want to get him in trouble.
Would you still do neurosurg if it paid as much/little as primary care?
 His salary would be in the negatives subtracting malpractice premiums.
His salary would be in the negatives subtracting malpractice premiums.Hi @neusu, you are amazing for answering these questions. It took me about 3 days to go from page 1 to 19, but you have helped so many people out (including answering various repeated questions with patience and politeness).
Here's my question:
How well do you think homosexuals are accepted in neurosurgery in these days by their co-residents, fellows, and attendings? I'm sure this will change as millenials fill residency positions, but I think the change will be rather conservative.
Do you think non-effeminate homosexual males will generally be more accepted than a more effeminate one? On this note, do you know any homosexual males or females in neurosurgery?
Is there a factor of machismo involved in work (like, say, a stereotypical surgeon or ortho) no matter whether male/female?
Any time!Thanks for responding!
I did a search for "international" on this thread before asking, but how hard is it to get a neurosurgery residency as an IMG? I've seen salaries from $180k to $500k. How much can a neurosurgeon expect to make.
In terms of problem solving/thinking, how does neurosurgery differ from neurology?
Thank you so much for taking the time to answer these questions.
Thank you. As a followup, how many neurosurgeons do you know that are IMGs?Obtaining a residency in the US as an IMG is exceptionally hard. The ones who are successful often spend a year or more at an institution and make inroads through that program. Overall, they tend to have statistics well above the mean for us grads (scores, publications, etc), and often, still do not match.
Salaries in neurosurgery vary widely depending on the practice model and practice location.
Neurologists and neurosurgeons deal with overlapping problems in many cases. Our diagnostic tool-set is very similar. That being said, we as surgeons generally split any patient we evaluate in to the categories of opeartive or non-operative.
Would you still do neurosurg if it paid as much/little as primary care?
First off I would like to voice my admiration for you for pursuing such a field of work.
Second, I was wondering what it is thought about the future of neurosurgery. Obviously nobody knows the future but I've heard people in other specialties (neurology, for example) cite what lies in the pipeline as an example of the change the specialty will undergo in the future. DBS? Rehabilitation? Cancer? Oligodendroglioma? I've heard that a lot of cases in neurosurgery have limited chance of getting better, do you think that will change in the future?
Study well, do well in class and score good marks which prepares you best for the MCAT. Do well on the MCAT. Try to get involved in research. Have a life outside of school so you are well rounded.
For what it's worth, you can match in to neurosurgery from any accredited medical school in the world. Coming from a top US allopathic school just makes it slightly easier. It remains, nonetheless, a lot of hard work and a bit of luck.
Were you an underdog? Did you struggle in undergrad?
Thank you. As a followup, how many neurosurgeons do you know that are IMGs?
I'm from NYC, I was wondering how difficult it is to secure a residency in urban areas that are popular? And for older graduates, would Neurology be the better route if the problem-solving aspect is the biggest interest? I know every person is different, but just from your experience would be helpful.
Thanks for the response! I'm talking about a person who won't start medical school until they are 30.I do know a few neurosurgeons who graduated abroad. The vast majority, however are graduates of US schools.
Popular urban areas are more difficult to secure a residency position. Some areas have more programs than others (e.g. NYC, Philadelphia compared to Miami, Phoenix). Neurology is generally a much more forgiving residency both in hours during residency and length of residency. How much older are we talking here?
There are 19 pages here and I don't have the time to see if it has been answered but here is my question. My medical school (about to start M3) does not have a Neurosurgery program nor a neurosurgery rotation. I already have my schedule (a mix of civilian and naval rotations) and I am pretty dead set on IM/General Surgery to specialize. As you can see in my name, I am really fascinated by cancer. I want to mix that with Neurology/Neurosurgery. Are there programs out there that I can apply to to do Neurosurgery and focus on NeuroOncology?
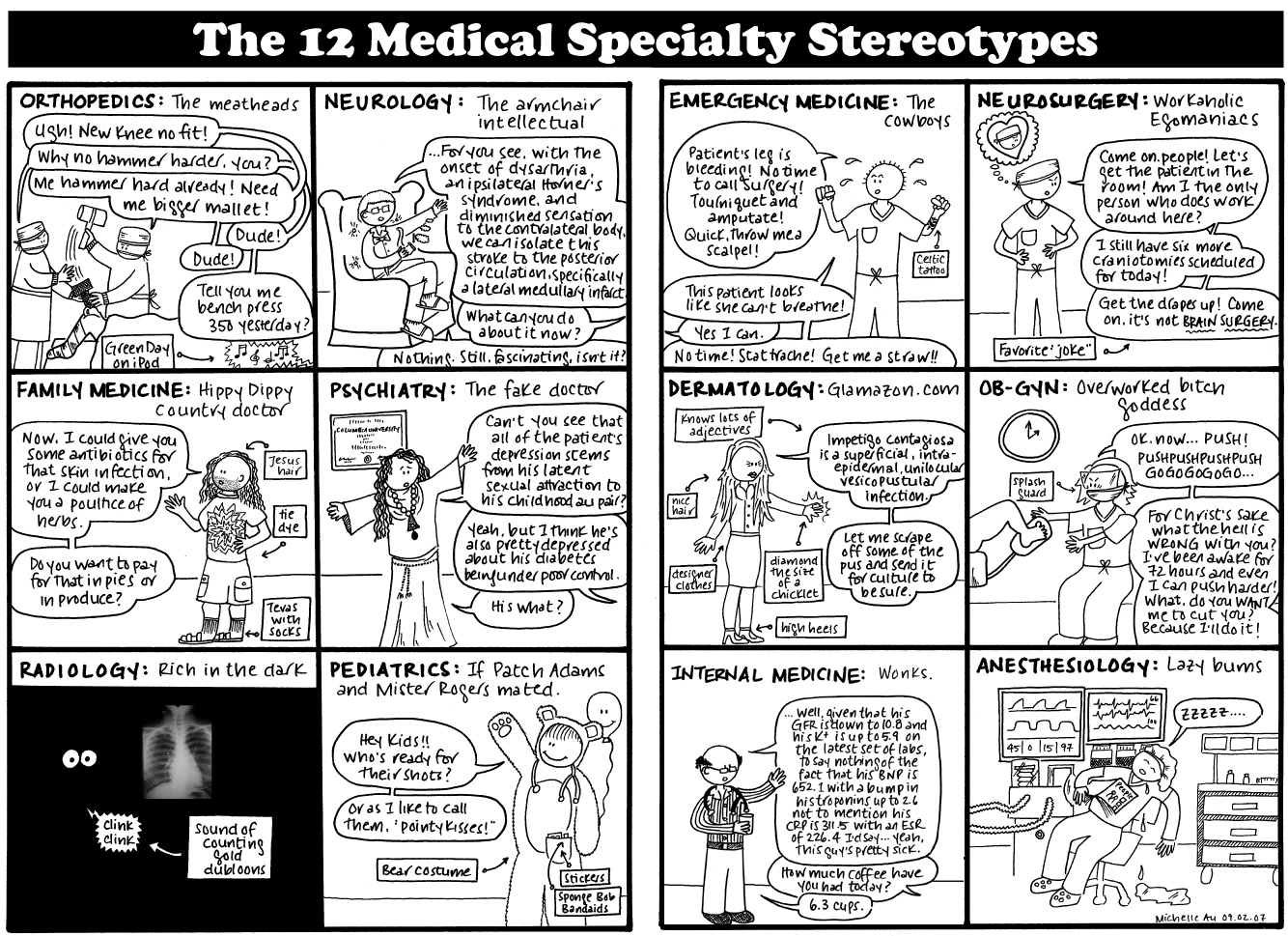
I would like to know some "funny stuff" about the different subspecialities within neurosurgery.
1) Do you see any personal traits/stereotypical personalities in the different subspecialities?
My (and I have very limited) experiencewould be something like:
Vascular: Hardcore guys. More like the general surgeons. Not so cerebral but enjoy the surgery part a lot.
Tumor: Often research-oriented too. Not the very best technicians and surgeons, but anyway get the job done and show a lot comittment to their patient population.
Pediatrics: Very cerebral people. Know a lot. Enjoying paying a lot of attention to details. Hardworking.
Functional: If they were not neurosurgerons they would be neurologists. Nice guys.
2) Could you share your experiences on what you think about the subspecialties? Pros and cons, a few lines of them
I'll have to think about this one and get back to you. When you say "funny stuff" do you mean peculiarities or a humorous generalization of each sub-specialty and the surgeons who practice therein or something else entirely?
Adjusting my perspective and goals has helped. I still find time to do the things I enjoy, just it doesn't define me in the way it did formerly.
Hi again,
Sorry, maybe I formulated it a bit odd. I would like to know if there are any clear stereotypical people in each subspecialty. Something along with what I had written from my very modest experience. Or.. if you find that there is no such thing as steretypical neurosurgeons in the different subspecialties.
For the second question, I would like to know some about where your interst lay in.. Maybe some words about the different specialty what you have enjoyed/disliked so far in your training.
How heavy is the work load?
This is more of a general residency question, and forgive me if it has been asked before. Does a residency program's prestige significantly affect an individual's ability to get hired and salary potential at a non-academic medical center? I'm fairly intelligent, but I know my limits and know that I most likely will not match into any top residency programs, especially in neurosurgery.
Thanks for the response! I'm talking about a person who won't start medical school until they are 30.
So, while there are more spots available in popular urban areas, it is overall more difficult because of the popularity/increased competition? How can I, as an IMG, make myself more competitive/stand out?
Just read the whole thread (took me a while!), thanks so much for doing this.
I'm applying to medical school this cycle and I'm looking to get some research experience before med school (hopefully!) starts in a year. I have never done bench research and my knowledge of lab techniques is limited to med school prerequisites (fetal pig?). I started looking at neurosurgery research at nearby med schools and I really don't think I'm qualified to even clean glassware for them... I do have pretty good experience in clinical research (psychiatry) and theoretical research (clin. psychology, with pub). Would you recommend trying to join a clinical research NS lab, since I'd be more helpful there? How do you make that first step in NS research with no previous NS experience?
Also, how much does NS research rely on animal models? Do you work mainly on rodents? This may not be a popular view among those in medicine, but I'd be really uncomfortable doing research using primates/dogs/cats/pigs.
Thanks!
Neusu, I see you're going in order but I think you perhaps skipped my question:
Thank you
Does having neuroscience-related research experience prior to medical school greatly enhance a residency application for neurosurgery?
Having a background in neuroscience research is helpful, but I would not characterize it as greatly helping a neurosurgery application. To the contrary, often, people with experience in neuroscience often equate their particular subsection of research to experience in neurosurgery as a whole. This, more often than not, is far from the truth.
While we do study neuroscience, and many neurosurgeons have basic or clinical science research (or both), there are many, many more non-neurosurgeon neuroscientists. Certainly, the techniques between these groups are similar. The focus and application of ideas often differ. Neurosurgery investigators are better poised to perform translational research with respect to devices and deliver mechanisms.
Research in any field will provide a leg-up provided you are productive and can discuss your project. Having a publication, or several, especially in high impact journals is important. Also, being able to explain your role within the project, both in a brief statement and in detail helps show you understand what you did and how you participated.
