- Joined
- Apr 3, 2007
- Messages
- 1,701
- Reaction score
- 722
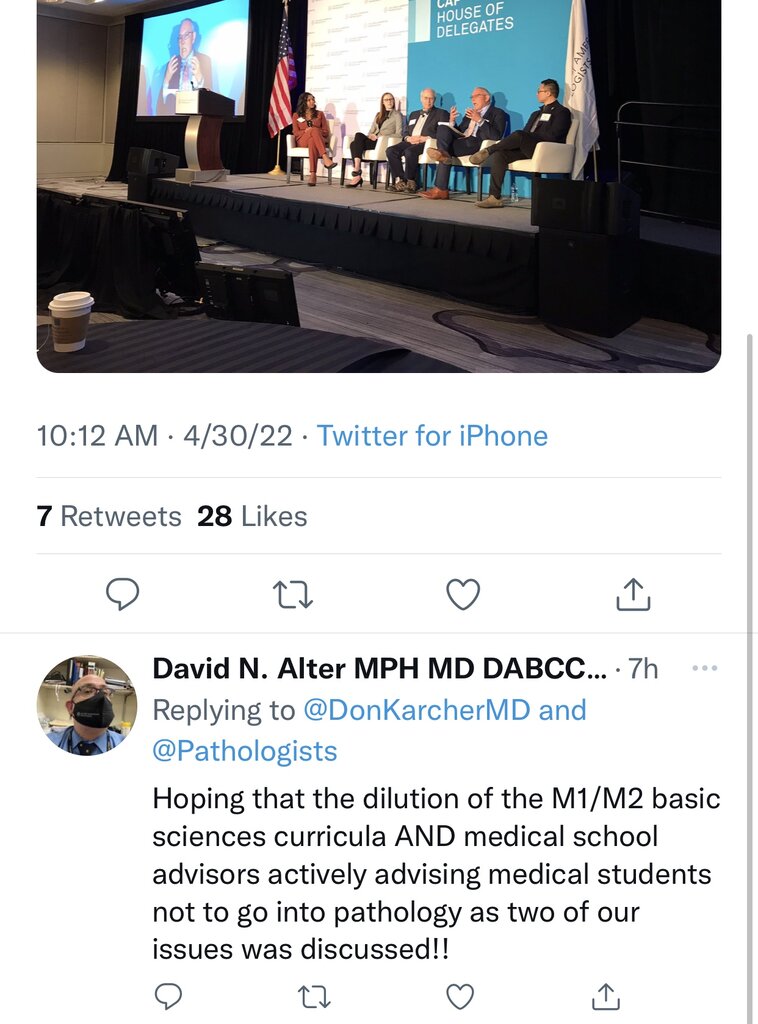
So there was a CAP Pathologist Leadership meeting over the weekend. Was anyone there who would like to talk about what was discussed during the workforce discussion?
Reading some of these tweets, a few things stuck out…
Apparently there is a pathology resident shortage? I LMAO at this. Dr Mills, around where I live there are 25-30 residents being put out every year (not including fellows). Jobs are very few. Few as in I can count the number of jobs on my one hand and you really think we need more residents? Really? Graduates, who want to stay in the area, are desperate to find jobs in the area because the market is tight.
You do know that Pathology is a haven for those IMGs who do not match into internal medicine to apply to right? Increasing the number of pathology residency spots will further degrade our field worsening both an already suboptimal job market and the quality of pathologists we graduate every year.
The barrier of entry of our field is approaching that of pediatrics and family medicine (if not already there) when it should actually be much higher considering the job we do.
Medical student advisors are recommending medical students not to go into Pathology? All of you medical students, is this the case at your schools? Hmmmm…I wonder why?
SERIOUSLY, WE NEED MORE PATHOLOGISTS?!?


Reading some of these tweets, a few things stuck out…
Apparently there is a pathology resident shortage? I LMAO at this. Dr Mills, around where I live there are 25-30 residents being put out every year (not including fellows). Jobs are very few. Few as in I can count the number of jobs on my one hand and you really think we need more residents? Really? Graduates, who want to stay in the area, are desperate to find jobs in the area because the market is tight.
You do know that Pathology is a haven for those IMGs who do not match into internal medicine to apply to right? Increasing the number of pathology residency spots will further degrade our field worsening both an already suboptimal job market and the quality of pathologists we graduate every year.
The barrier of entry of our field is approaching that of pediatrics and family medicine (if not already there) when it should actually be much higher considering the job we do.
Medical student advisors are recommending medical students not to go into Pathology? All of you medical students, is this the case at your schools? Hmmmm…I wonder why?
SERIOUSLY, WE NEED MORE PATHOLOGISTS?!?
Last edited:

 .
.