- Joined
- Oct 30, 2011
- Messages
- 260
- Reaction score
- 37
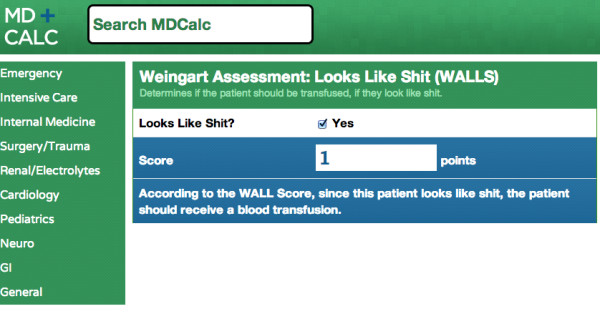
During trauma resuscitation is any attention paid to hemoglobin levels [i.e. "Hb is 10.0 so don't transfuse PRBC"], or is the decision exclusively about hemodynamics and circulation exam?
I assume that a low Hb would indicate transfusion requirement, so my main question is would a normal Hb ever prevent transfusion?
Thanks!
I assume that a low Hb would indicate transfusion requirement, so my main question is would a normal Hb ever prevent transfusion?
Thanks!