- Joined
- Dec 1, 2006
- Messages
- 1,312
- Reaction score
- 2
Can anyone think of any reason, other than a lab error, that a hemoglobin might be elevated while the hematocrit is decreased, or vice versa?
Can anyone think of any reason, other than a lab error, that a hemoglobin might be elevated while the hematocrit is decreased, or vice versa?
Can anyone think of any reason, other than a lab error, that a hemoglobin might be elevated while the hematocrit is decreased, or vice versa?
Hemoglobin is calculated based on the hematocrit. They are the same thing. There are "crit" people and there are "hemoglobin" people. Crit people think in 3s, globin people in 1s. In general, 1 hemoglobin = 3 Hematocrits. The calculation is not exactly 1:3, but is close enough such that within normal variation it doesn't matter which you use, because they are the same number, they are the same thing, just one is measured and the other calculated.
There are definitely plenty of reasons they can vary independently of each other. That's why you need the other RBC indices (MCV, MCH, and MCHC) to help you evaluate reasons for this. When you're looking at the ratio of those two you're talking about MCHC, hgb*100/hct.
You probably most of this already but to start at the beginning...
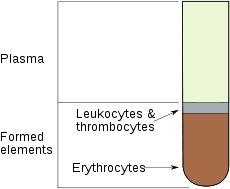
Hct is a measure of how much space in the blood is composed of red cells as opposed to plasma or white cells. It's calculated on most analyzers based on the number of RBCs and volume of red cells (MCV). So if number of cells decreases or cell sizes decreases, ie they take up less space, the hct decreases.
Hgb is going to be function of production and loss of hgb molecules. If you have the same amount produced but you're kicking out larger or smaller cells you'll get a discrepancy. That's why anemias are often described in terms of both cell size (normocytic, macrocytic, microcytic) and pallor (normochromic, hypochromic, hyperchromic).
The hematocrit (Ht or HCT) or packed cell volume (PCV) or erythrocyte volume fraction (EVF) is the volume percentage (%) of red blood cells in blood. It is normally about 45% for men and 40% for women.[1] It is considered an integral part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count, and platelet count.
If the concentration is below normal, this is called anemia. Anemias are classified by the size of red blood cells, the cells that contain hemoglobin in vertebrates. The anemia is called "microcytic" if red cells are small, "macrocytic" if they are large, and "normocytic" otherwise.
Hematocrit, the proportion of blood volume occupied by red blood cells, is typically about three times the hemoglobin concentration measured in g/dL. For example, if the hemoglobin is measured at 17 g/dL, that compares with a hematocrit of 51%.[61]
The Mean...
I don't know how Hb is assayed in the blood, but assuming it can't differentiate between free and intracellular Hb, one would guess that acute massive RBC lysis would cause a normal Hb with decreased crit
