- Joined
- Sep 16, 2008
- Messages
- 491
- Reaction score
- 220
SDN Anesthesia Hivemind--
What is your threshold for gaining large-vessel arterial access in patients with significant (or significant anticipated) vasopressor requirement?
There's obviously some (albeit not a huge volume) of data showing a significant discrepancy between radial arterial pressures and "central" arterial pressure (usually femoral). Here's a nice PulmCrit review: PulmCrit: A-lines in septic shock: the wrist versus the groin , and I've attached a 2005 paper looking at fem vs radial in liver transplantation.
I had a case from a while ago where the patient came to the OR on 18 of norepi and 0.08 of vasopressin, so I thought there was a very reasonable expectation that vasopressor requirement would get worse before it got better. I placed a brachial art line and there was a ~50 point difference in SBP, though only ~10-15 point MAP difference.
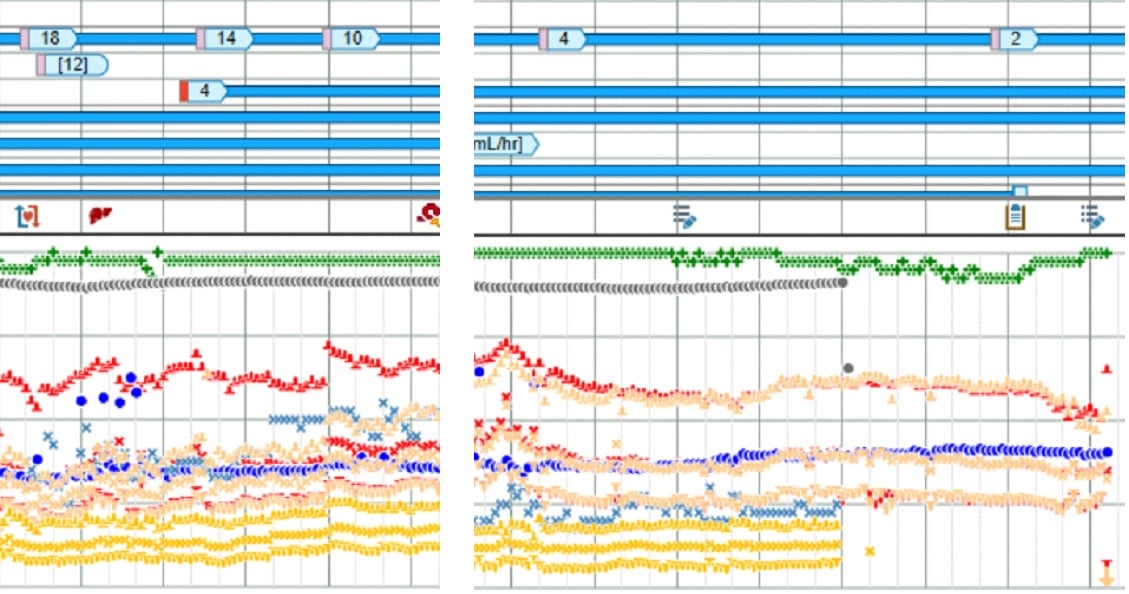
By the end of the case with the patient basically off vasopressors, the two arterial lines had equalized as seen in the second image.
Obviously large vessel arterial access carries more complications, esp in sick patients (sorry CCF, but I don't believe your data). So what's your practice for placing fem/brachial lines? Does the brachial actually count as "central", or do you prefer axillary? Do you think it makes a difference in the patient's overall morbidity? My thought in these extremely low SVR patients is that the extra vasopressor required to get 10 points to achieve the MAP goal could have a significant negative impact on tissue perfusion, but I have absolutely zero data to back that up.
What is your threshold for gaining large-vessel arterial access in patients with significant (or significant anticipated) vasopressor requirement?
There's obviously some (albeit not a huge volume) of data showing a significant discrepancy between radial arterial pressures and "central" arterial pressure (usually femoral). Here's a nice PulmCrit review: PulmCrit: A-lines in septic shock: the wrist versus the groin , and I've attached a 2005 paper looking at fem vs radial in liver transplantation.
I had a case from a while ago where the patient came to the OR on 18 of norepi and 0.08 of vasopressin, so I thought there was a very reasonable expectation that vasopressor requirement would get worse before it got better. I placed a brachial art line and there was a ~50 point difference in SBP, though only ~10-15 point MAP difference.
By the end of the case with the patient basically off vasopressors, the two arterial lines had equalized as seen in the second image.
Obviously large vessel arterial access carries more complications, esp in sick patients (sorry CCF, but I don't believe your data). So what's your practice for placing fem/brachial lines? Does the brachial actually count as "central", or do you prefer axillary? Do you think it makes a difference in the patient's overall morbidity? My thought in these extremely low SVR patients is that the extra vasopressor required to get 10 points to achieve the MAP goal could have a significant negative impact on tissue perfusion, but I have absolutely zero data to back that up.

