- Joined
- Sep 15, 2011
- Messages
- 459
- Reaction score
- 212
50's cardiac history on warfarin.
had two successful mbb, and then lumbar RFA 2 weeks ago.
post procedure meeting - 2 weeks - complained of severe pain in right low back with hip flexion weakness, i got stat MRI
this is what the MRI shows
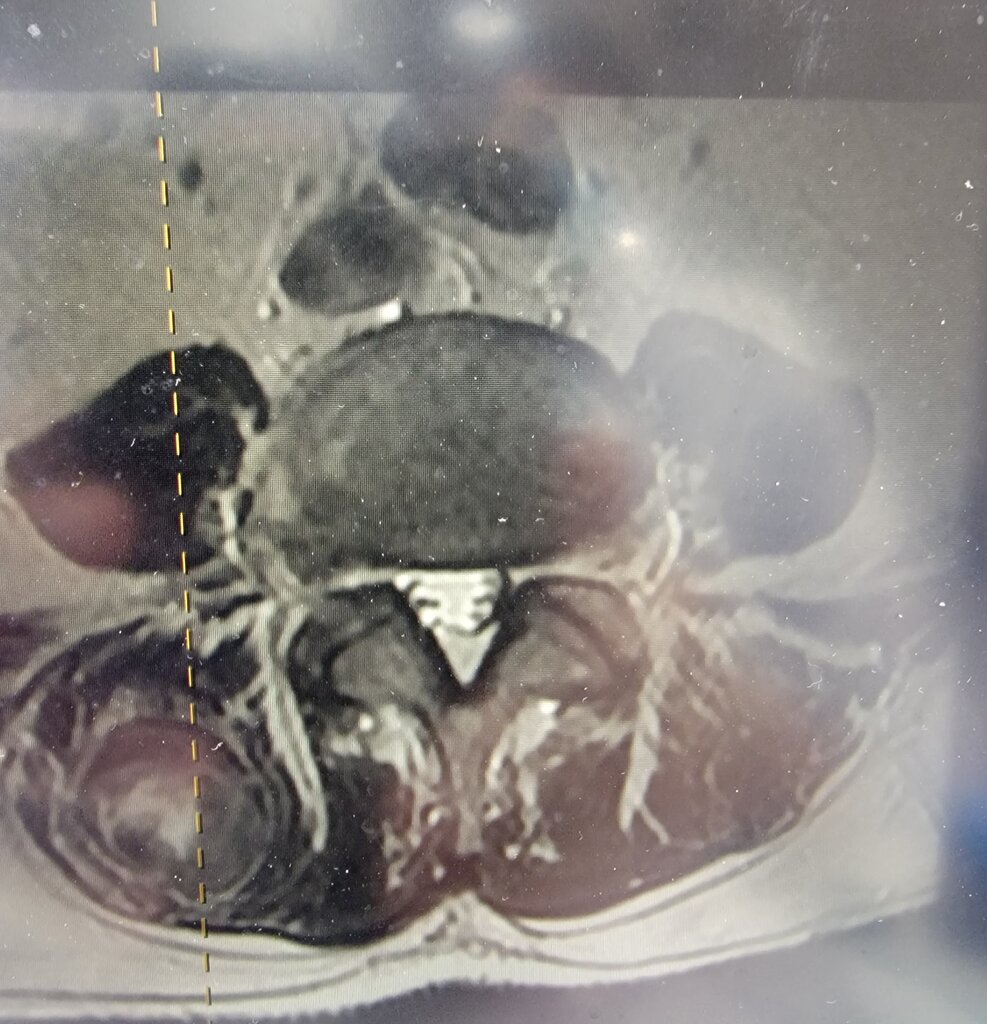
3cm hematoma in the paraspinous muscles. no impingement in neuroforamen/no hematoma in epidural space. of note, he does have a known 5cm AAA. i think the hematoma is causing the pain - any thoughts? how would you proceed? drain it? leave it until it gets absorbed?
had two successful mbb, and then lumbar RFA 2 weeks ago.
post procedure meeting - 2 weeks - complained of severe pain in right low back with hip flexion weakness, i got stat MRI
this is what the MRI shows
3cm hematoma in the paraspinous muscles. no impingement in neuroforamen/no hematoma in epidural space. of note, he does have a known 5cm AAA. i think the hematoma is causing the pain - any thoughts? how would you proceed? drain it? leave it until it gets absorbed?

