The role of RT in lymphoma is decreasing in the past years, but the reason are not "evil" hematologists. It's evidence as well.
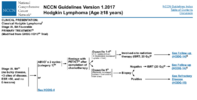
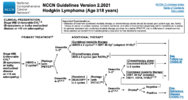
HD17 recently showed that consolidation with RT can be omitted if interim-PET-negative after 2x BEACOPP esc followed by 2x ABVD in early unfavorable Hodgkin's.
Flyer showed that giving 4x R-CHOP is enough for early stage DLBCL without any RT. The
Miller-approach of 3x CHOP + RT was preferred by many over 8x CHOP. Then R came along and the number of CHOP-cycles dropped to 6. But when the difference now is only one more cycle of R-CHOP which will allow you to skip RT, can you blame the hematologists for "pushing" the RT-free option?
In early favorable Hodgkin's things are less crystal clear. Omitting RT there will lead to an excessive risk for recurrence, but I've seen many patients opt to drop RT, even if that means 7-8% higher recurrence risk. On the other hand, if the volume is big and right in the mediastinum and you are an 19 year old young woman, what would you rather accept? 7-8% higher risk of recurrence by omitting RT or 3-5% (?) higher risk of RT-induced breast cancer? Protons can help there, but that's it....
One possible outlook will be RT in the setting of CAR-T-therapy. But still, there's a lot of work to do there!