- Joined
- Dec 2, 2011
- Messages
- 1,487
- Reaction score
- 3,011
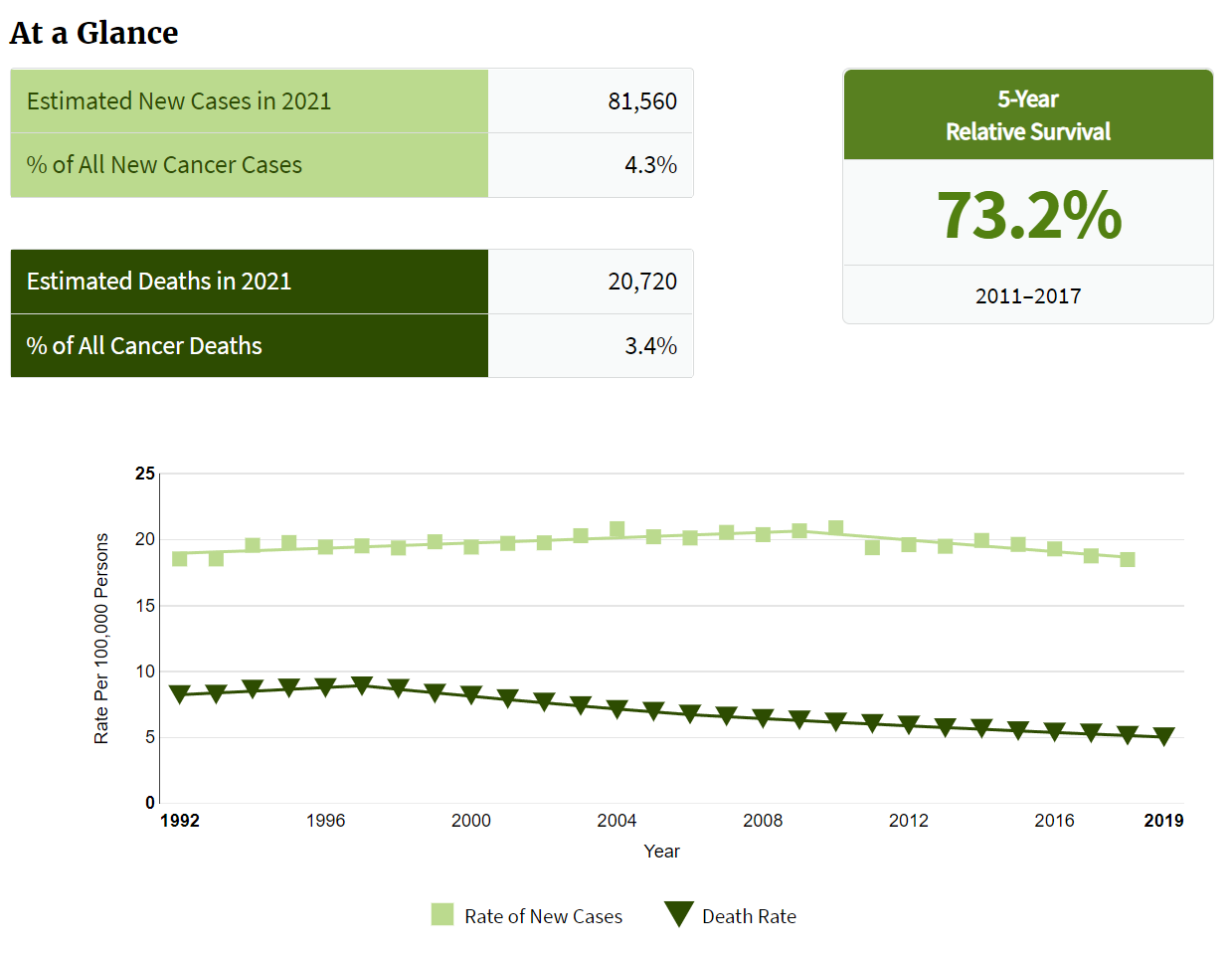
Just goes to show for what is a "rare" cancer. Only about 13K cervical ca cases/year in the U.S. Assume 75% are brachy candidates. So about 10K new cerv brachy pts a year for the entire country. This would yield about 2 cervical cancer patients per rad onc per year in the U.S. So if you're seeing 6 unique a month, or 72 a year, that means you see roughly 30 times more cervical cancer patients than the "average" rad onc. There's *significant* variation in case loads and case makeup from rad onc to rad onc in the U.S. Emphasis on significant. This is what happens in oversupply!
That and there are only 2 sites in our midwestern state that do T&Os and I am the only one that does interstitial. Half of these people do their EBRT at other centers. Also, I should clarify, 6-8 unique GYN patients get implanted. Most are cervical, but probably a third are either vaginal primary or cuff recurrences. Might have oversold the number of cervical patients a bit in my first post.