- Joined
- Mar 1, 2009
- Messages
- 35
- Reaction score
- 3
Do you guys use a stylet while intubating routinely for your cases? Just curious what folks are doing in the real world...
Do you guys use a stylet while intubating routinely for your cases? Just curious what folks are doing in the real world...
I do. It's easy to pull if you don't need it, and it saves me a DL if I find I do need it.
The main downside to the stylet is because the stiffness increases the risk of tracheal perforation if you are not gentle, or more importantly if there is abnormal tracheal anatomy. That is why I pull it once the tip of the tube is between the cords.
I do. It's easy to pull if you don't need it, and it saves me a DL if I find I do need it.
The main downside to the stylet is because the stiffness increases the risk of tracheal perforation if you are not gentle, or more importantly if there is abnormal tracheal anatomy. That is why I pull it once the tip of the tube is between the cords.
Do you guys use a stylet while intubating routinely for your cases? Just curious what folks are doing in the real world...
Not all the time. I will load one if I have any concerns about a possible difficult intubation.
If not using a stylette I'll form the ETT in a circle while setting up my room, inserting the Murphy eye end into the circuit adapter end, and leave it like that in the wrapper while I go get the patient. After detaching the two ends the ETT will maintain a slight fishhook appearance for a few minutes.
I do. It's easy to pull if you don't need it, and it saves me a DL if I find I do need it.
The main downside to the stylet is because the stiffness increases the risk of tracheal perforation if you are not gentle, or more importantly if there is abnormal tracheal anatomy. That is why I pull it once the tip of the tube is between the cords.
is there data on this? i always have one in. it does not take an extra person to pull it out 😕.
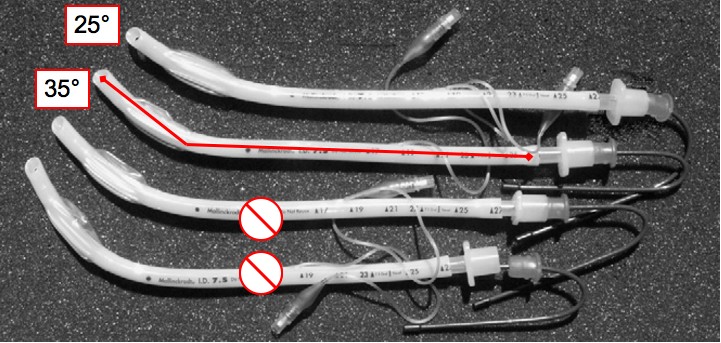
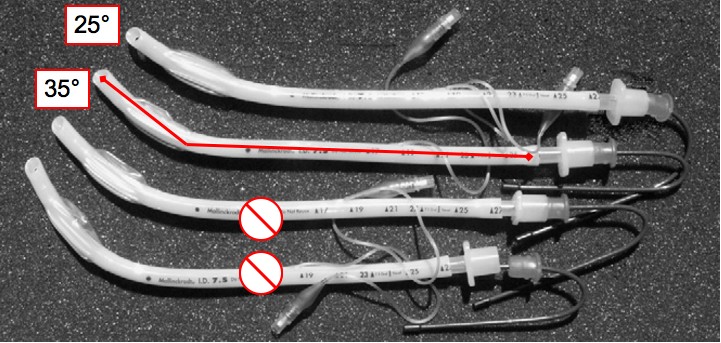
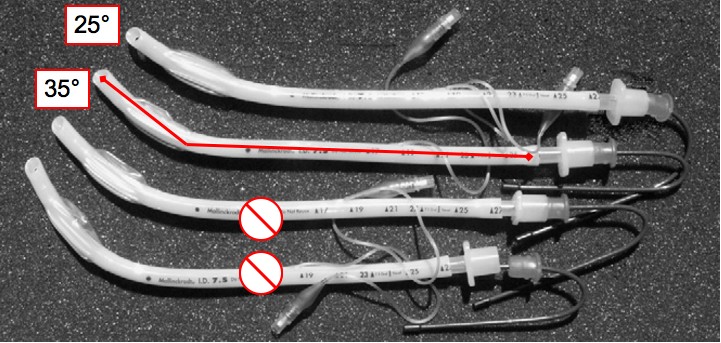
i find that a lot of the trainees I work with have gotten used to bending a sharp angle in their ETT/stylet combos (see bottom example - even worse sometimes!) which is totally unnecessary (and possibly dangerous) for all but the most anterior airways. I put the tiniest little bend in it but I typically want it fairly straight.


is there data on this? i always have one in. it does not take an extra person to pull it out 😕.
i find that a lot of the trainees I work with have gotten used to bending a sharp angle in their ETT/stylet combos (see bottom example - even worse sometimes!) which is totally unnecessary (and possibly dangerous) for all but the most anterior airways. I put the tiniest little bend in it but I typically want it fairly straight.
1) You need to update your avatar. There is no stylet.
2) I'm not sure what advantage there is to placing a stylet into a tube that basically mimics the curvature of the native tube.
I've got no issues for those who choose to not use a stylet routinely; but, I've had airways were a stylet was crucial to a successful intubation. At least several times a week I load up a stylet for a CRNA who couldn't pass the ETT without one.
Any antincipated difficult airway should have a stylet in the ETT; some say even the routine airway in non edentulous patients should get a styleted ETT. Why subject the patint to more trauma than needed with multiple larygoscopies? Again, I'm always happy to remove a stylet (satin slip) and save it for another patient. Of course, I've had CRNAs ask me to remove the stylet only to then request I put it back when they fail to pass the ETT on the first attempt.
I agree. I stylet every RSI, without question. And I stylet most that I think will be difficult, or at least have it on the gas machine.
I think comparing your practice with CRNAs to a trained physician asking for their own personal practice is apples to oranges. I also think of stylets like I think of oral airways. Crutches most of the time. I believe residents should begin their training using both, because they need to develop some confidence and basic skills to function somewhat independently. But I can bag-mask 95% of my teeth-wielding patients without an adjunct. And I can intubate 98% of my standard airways without a stylet. I believe both of those devices tend to allow practitioners to forge ahead without optimizing chin lift and mask seal skills, or DL and head positioning skills. A styletted tube can make it into places with Gr 3 views. Without that, I am often forced to optimize my positioning, etc.
I'm sure they say the same things as you over at Noctor.org; they never need a stylet or an oral airway (oral airways are used primarily in edentulous patients in my practice).
This hasn't been my observation and I bet a study of CA-3 Residents across several thousand intubations would show stylets decrease the number of laryngoscopies required for intubation. As for most things this is user dependent; but, I'd rather have a pre-loaded ETT ready to go then fish around for one when needed.
I at least encourage Residents to make certain there is a stylet ready and available for every intubation. You never know when you are going to need one until you need it.
Failing to prepare is preapring to fail.
-UTSW
I really could give a **** what they say over there. I don't visit. And I don't compare my intubating skills, or yours, to any of them. Because I am confident I can perform better than them in basically any clinical situation. I'm not the best on the block with everything, but I feel pretty good about my ability to drop a tube into a trachea.
And I really don't care about a study comparing stylet use with a batch of CA-3s. I'm not a CA-3, and I have proven to myself that I possess the skills to intubate these patients without a stylet. Period. I also have stated that I know when a stylet is useful, and I use it appropriately.
And I absolutely 100% agree that every resident, and every practitioner, should make sure there is a stylet available. That should go without saying.
Easy there Bert. The CRNAs I am referencing in my posts have an average experience level of 8 years out of training. They are not newly minted grads. But, I know most of them do compare themselves to Anesthesiologists and follow our examples. Hence, 90% of them don't start with a stylet in the ETT; some don't even bother checking that there is a stylet in the room or another intubating blade which works.
When I read threads like these it reminds why I'm glad the ASA sets standards in practice. From U/S to Pulse Oximetry the ASA has enhanced patient safety (IMHO).
If it was up to individual practitioners too many things would not be routinely used in practice and many patients across the USA would suffer as a result.
Is there a standard stating I must have a stylet in my tube?
I know it's great to think there is some ideal way to practice, which, if we all followed it, there would be no adverse events. That's not reality. Every patient is different, every practitioner is different.
If you are trying to dictate my choice of stylet, what next? Tell me I should be using a Mac blade on every patient?
Easy there again Bert. I don't think a discussion about stylets warrants such heated debate. I was making a bigger point about safety and standards in practice. The fact that a patient gets 2-3 laryngoscopies because a provider's ego gets in the way doesn't rise to that level.
There is no standard for stylets or type of intubating blade for routine cases requiring General endotracheal intubation.
I'm still glad the ASA does set standards on major issues like pulse oximetry, EKG, ETCo2, etc. or we would be debating those as well.
And I'll settle down when you stop comparing me to your CRNAs.
My intent was not to compare you to my CRNAs. They like to compare themselves to you. Do you see the difference there? Since you don't use or need a stylet in the ETT then they believe (erroneously I might add) they don't need one either.
You set the standard and they follow.
This may surprise some folks, but I stylet every tube with a fairly steep bend. My average time from entering the the OR to having the airway secured is just under five minutes. Sometimes three and rarely do I go over 5 minutes. I can't afford to waste an attempt because I needed a stylet and didn't have it. I have the luxury of having a circulator assigned to assist me until the airway is secure so removal is not an issue. Induce, DL, place the tip through the cords and ask the circulator to remove the stylet. Advance tube and reconfirm correct position. Remove laryngoscope.
I rarely need it, but when I do, I don't have to withdraw, place stylet and re-DL. I use the satin stylet.
- pod
Ok for those who stylet routinely, how often does it happen that you have to DL x2 because the curve on the stylet was not appropriate?
If the patient in in the sniffing position the line from the mouth to the trachea can be very strait thus any curve you would have on your tube would make it hard to intubate.
There are a lot of factors that come into play in how you approach the airway, patient morphology is one of them and varies with where you practice.
As Bert said i know when i need one and when i have a difficult airway i prefer to go strait to the bougie. Overall i need these tools very rarely so i don't feel the need to bother with systematic use.
Ok for those who stylet routinely, how often does it happen that you have to DL x2 because the curve on the stylet was not appropriate?
If the patient in in the sniffing position the line from the mouth to the trachea can be very strait thus any curve you would have on your tube would make it hard to intubate.
There are a lot of factors that come into play in how you approach the airway, patient morphology is one of them and varies with where you practice.
As Bert said i know when i need one and when i have a difficult airway i prefer to go strait to the bougie. Overall i need these tools very rarely so i don't feel the need to bother with systematic use.
The question is how often do you perform a second DL which could be avoided by having a stylet preloaded and do you believe avoiding that second DL warrants the routine use of that stylet.
Why? If the numbers are the same you have no ground to stand on...
So how often do you do multiple DLs with a stylet?
I practice in an ACT with CRNAs. I believe stylets reduce trauma and the number of DLs..
I rarely do multiple DLs with a styleted ETT; I usually intubate more frequently than I would like and use a Miller blade with a styleted ETT.
And if you are able to rotate the styletted ETT all sorts of ways to make it in the hole, realize you can do the exact same thing with an empty tube.
This may surprise some folks, but I stylet every tube with a fairly steep bend. My average time from entering the the OR to having the airway secured is just under five minutes. Sometimes three and rarely do I go over 5 minutes. I can't afford to waste an attempt because I needed a stylet and didn't have it. I have the luxury of having a circulator assigned to assist me until the airway is secure so removal is not an issue. Induce, DL, place the tip through the cords and ask the circulator to remove the stylet. Advance tube and reconfirm correct position. Remove laryngoscope.
I rarely need it, but when I do, I don't have to withdraw, place stylet and re-DL. I use the satin stylet.
- pod
Come on now Bert, it's fine for you to disagree with the routine use of a stylet, but you know that's just not true.
You either know that the tube is in or you don't know, there is no think that it is in. Anesthesiologists get in trouble because they fool themselves and think that the tube is in. Confirm it. Don't remove the laryngoscope immediately upon placing the tube. Place the tube, then take another look. Is the tube still between the cords? Then the rest doesn't matter. Even if they are so bronchospastic that there are no breath sounds and no EtCO2, you KNOW that the tube is in. But be honest with yourself if you don't know for sure, then you need to rely on other methods of confirming tube placement.
What I am saying is that if you find that the natural curve of the ETT is not aligning well with the cords, you can rotate the tube, bringing the angle down, and slide it in. I am not making this up. Rotating the tube alters the position of the tube tip.
If I find that I need a little more anterior bend, I can push the tube against pharyngeal structures, get a fulcrum to change the tip angle, and advance. I'm not making this **** up, I do it every day.
I should add that I am not critical of Anesthesiologists that do not use a stylette for every intubation.
You're selling out? 😉
You're selling out? 😉
... and it costs 2 dollars.
The pennypinchers around here clean and re-use stylets so the cost is essentially $0.
I put one in every tube - just don't see the downside.
