Healthcare in America in 2022 is wild. American RadOnc is wild.
Radiation was discovered, we found out it could kill things. We first used the Spicy Rocks™ to kill things, then we made machines. We could kill things without touching people, like in the comic books.
Simultaneously, some teachers in Dallas figured out they could pool their money together in case they got sick and needed to go to the hospital. This was back in the day when people knew "medicine" wasn't synonymous with "insurance".
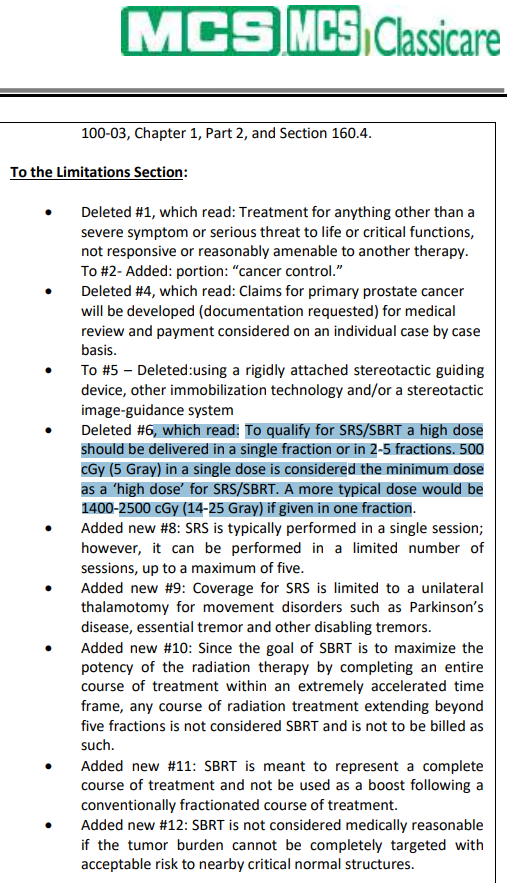
Things snowballed, as they often do. The iPhone was invented. We figured out how to get Spicy Rock™ level precision with our machines. Insurance somehow came to mean medicine, and folks with oily mustaches and three-piece suits learned how to amass fabulous wealth from other people getting sick.
But only the right people are allowed to amass wealth. Somebody made a graph once which showed some RadOnc doctors made more money from the better radiation. Doctors are allowed to be in a certain range of wealth, but they need to know their place. In order to appease the oily mustache Overlords, we engaged in grassroots self-flagellation, hoping we could make ourselves bleed so badly the government couldn't recognize our hemorrhaging faces. You think face recognition struggles with a mask? You should see what happens with 3 inches of congealed blood.
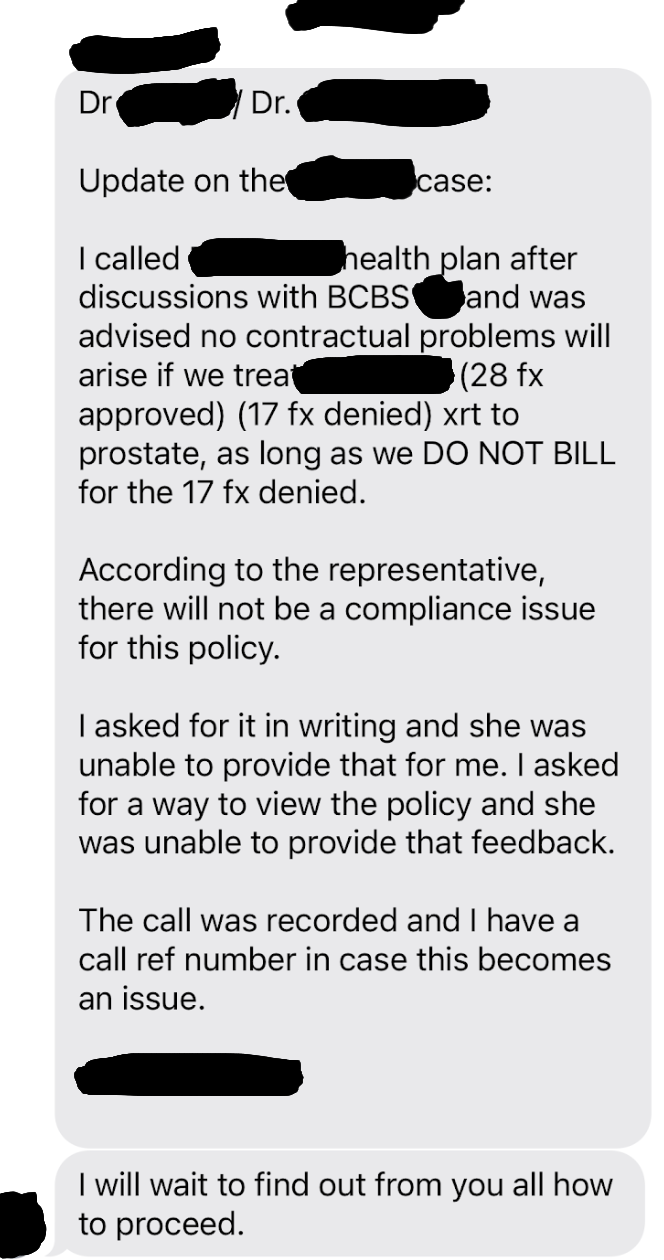
So here we are, making this thread, asking this question. A doctor wants to do a treatment. Insurance says no no no, we practice the medicine 'round here, not you, friendo. The doctor says fine, I'll do my treatment for the lesser reimbursement of the other treatment, sound good?
Chaos. Fraud. Violence. Entropy.
If you insist on curing cancer, you buffoon, you must do it our way, for our price. You went to medical school? What's your point? You want a pat on the head? Get back to work, and make sure you use the 2022 CPT codes, not the 2021 codes, or we'll audit you into the ground.