- Joined
- May 27, 2020
- Messages
- 43
- Reaction score
- 392
It has been a while since I have jumped on SDN and was hoping to gain additional vantage points and perspectives on a hot topic on SDN. I realize there are many posts/threads, papers, tweets, etc on this, but wanted to try to get the discussion going in a different way than I have seen (if I missed it please shoot me a link to the relevant thread). The impetus for this post is that I am speaking as a panel member at the upcoming SCAROP meeting in a few weeks on the issue of interest in our field/applicant numbers.
Normally I start any project with identifying the problem clearly and concisely, and then doing a root cause analysis to the upstream and downstream effects, causes, correlations to understand how to study and fix it. I am struggling to identify and appropriately characterize what the issue is exactly. I do not mean this to say there is no issue, but I am struggling to consicely convey what the problem is that gets discussed so passionately. This 1st step is so critical as you cant solve something, or even appropriately study it if you cant define it.
Many discuss the concept of this problem frequently, but what is it exactly?
-Is it reduced interest in our field? Some would say that interest is still there of those that apply, so it cant be just interest. Applicant numbers are reduced, so is it general interest perhaps is reduced? Is lack of more broad interest itself a problem? Is it a lack of positivity in our field or promotion of our field the problem? Furthermore, is reduced applicants an actual problem for a field? Reflexively many people say yes, but why? Reduced applicants means fewer residents to train (assuming SOAP did not occur) and this may be natural market forces balancing of supply and demand. However, as SOAP does occur, then is the problem we have people entering our field without prior radonc interest (or as much interest)? I then ask what is the problem that this results in? I did not know about radonc until a few months before I applied and never did an away rotation. My appreciation for radonc grew stronger over time, so I am not convinced that it is a problem in and of itself. Or is it the caliber of people who SOAP in not sufficient? I again challenge this as does having someone publish a nature paper with a Step 1 score of 270 from Harvard mean they will be a better clinical radonc than someone who did no research in med school, got a 220 from a state school? Not sure that this is the actual problem either.
-Is it the change of the job market as a result of the changes in healthcare (consolidation of practices, fewer and fewer solo practices, etc)? What is the unique problem that radonc faces that other specialties do not with these changes? Jobs are more now than ever part of bigger and bigger centers/companies and what was independent practices are now community affiliate positions. Is this the problem? This is happening across healthcare, so is this unique to radonc?
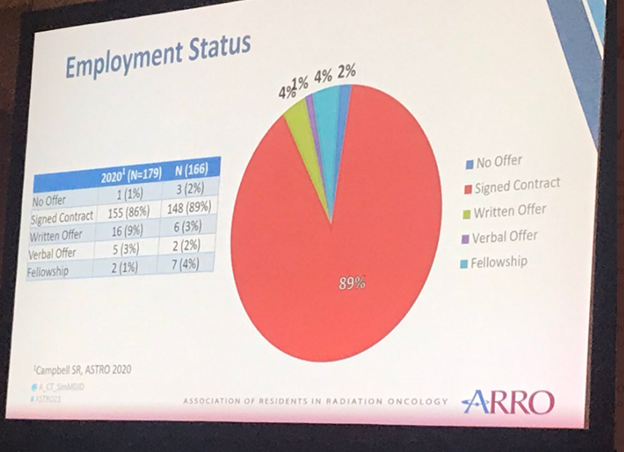
-Is it that residents are graduating and they are not getting a job after years of school, training, and debt? What is the best data for this to graduates truly not having any open positions to apply to. I say this as right now in Northeast Ohio alone I know of one group using a locums looking to hire a permanent doc, another using 3 locums trying to find 2-3 permanent positions, and another using 2 locums that needs 3 permanent docs. These are all centers not part of my institution. I have hired 8 physicians in 12 months and am recruiting 6 more. So is it that there are in fact jobs, but they are not the types of jobs people want (community vs main or solo vs multi-provider practice or academic vs non-academic or salary level or research or city vs rural or middle america vs coasts)? Totally understand not everyone wants to move to some of these centers in the rural midwest, or the environment is not what they want, but they are jobs. This difference matters in order to address the issue. Or is it number of jobs and the types of jobs? Is it a mismatch in we have tried to attract hyper academic, many MD/PhDs, to a market that supports having very few of them and so there is a mismatch of applicants wants and job availability? If we recruited mainly people who wanted to be community radoncs across the country would we have the same discussions?
-Is it the expansion of medschools/slots and residency programs/slots and this goes back to is there truly an oversupply and not enough demand? Or the demand is there does not match the interests of the applicants (ie tons of people graduating in Cali and NYC but jobs are needed in middle america)?
-Is it a DEI issue (or at least in part)? Our applicant pool is dominated by non-URM males so we are missing out on hundreds (or thousands) of women and URM that are applying to derm, radiology, etc. While this should absolutely be addressed and likely a contributing factor, it doesnt appear that the diversity in radonc is rapidly declining to explain the sudden change from when I applied to radonc in 2010 and by 3 years after I graduated in 2018 applicant numbers seemed to be dropping. If anything I thought I saw in recent papers some improvements in some components of diversity (at least gender) in radonc faculty.
-Is it a generational (I am a millennial technically too) or a manifestation of social media in that issues can now be brought out into the light to mass audiences more easily? I hope this audience can appreciate at times there has been disrespectful and unproductive comments on SDN, twitter, etc, often highly personal, about how bad they believe radonc is and people should run from it....that of course would impact potentially interested people in radonc. Perhaps this is the goal of these people, to sound the alarm to whatever the problem is and help these individuals go into another field. However, data will show that most other providers in medicine work longer hours for less pay and debatable have less impact as curing or palliating cancer...I realize many may disagree but I can tell you that I as Chair talk with many other Chairs whose faculty make far less and work more. However, I would think the generational and social media impact would impact all specialties fairly equally. So what appears unique to radonc? Or is this unique to radonc?
-Is it declines in private/community practice compensation with healthcare consolidation? In most academic university centers salaries have gone up (they were in the low $200k at U of M for new grads 10+ years ago and now are >$300k...I realize inflation is brutal recently but salaries went up). However, the days of private groups owning their equipment and getting the tech revenue is uncommon now, so the >$1m salaries (more than even almost every single Chair makes in the country based on SCAROP data) are hard to come by. However, salaries have tanked in dermatology (my wife is one and our family friend who just retired at 70yo from derm cleared $1m a year easily much of his career and now most derms (not all) make $250-400k...same major declines in general surgery, radiology, etc. So is this unique to radonc?
These are just some examples, but I would genuinely appreciate people who often write passionately about the decline of our field on this forum, and what the core problem is. Of course it is multi-factorial the cause, but what is the problem. This should be able to be clear and concise. Again, the causes and effects will be complex, but how would you state what the problem is in 1 short sentence.
I realize I am entering the lions den and I have read many of the incredibly negative and frankly disrespectful threads about me or my friends on SDN from people that have minimal to no personal knowledge or context to the things they write about. Not sure peoples motives for personal attack or how I have wronged them in my short career as faculty (~6.5 years)....but my name is Daniel so I hope my mom and dad were right giving me that name as the den has been entered!
If you would like for your anonymous voices to potentially be heard by the academic chairs across the country in Washington DC, let it rip.
Thanks
Dan
Normally I start any project with identifying the problem clearly and concisely, and then doing a root cause analysis to the upstream and downstream effects, causes, correlations to understand how to study and fix it. I am struggling to identify and appropriately characterize what the issue is exactly. I do not mean this to say there is no issue, but I am struggling to consicely convey what the problem is that gets discussed so passionately. This 1st step is so critical as you cant solve something, or even appropriately study it if you cant define it.
Many discuss the concept of this problem frequently, but what is it exactly?
-Is it reduced interest in our field? Some would say that interest is still there of those that apply, so it cant be just interest. Applicant numbers are reduced, so is it general interest perhaps is reduced? Is lack of more broad interest itself a problem? Is it a lack of positivity in our field or promotion of our field the problem? Furthermore, is reduced applicants an actual problem for a field? Reflexively many people say yes, but why? Reduced applicants means fewer residents to train (assuming SOAP did not occur) and this may be natural market forces balancing of supply and demand. However, as SOAP does occur, then is the problem we have people entering our field without prior radonc interest (or as much interest)? I then ask what is the problem that this results in? I did not know about radonc until a few months before I applied and never did an away rotation. My appreciation for radonc grew stronger over time, so I am not convinced that it is a problem in and of itself. Or is it the caliber of people who SOAP in not sufficient? I again challenge this as does having someone publish a nature paper with a Step 1 score of 270 from Harvard mean they will be a better clinical radonc than someone who did no research in med school, got a 220 from a state school? Not sure that this is the actual problem either.
-Is it the change of the job market as a result of the changes in healthcare (consolidation of practices, fewer and fewer solo practices, etc)? What is the unique problem that radonc faces that other specialties do not with these changes? Jobs are more now than ever part of bigger and bigger centers/companies and what was independent practices are now community affiliate positions. Is this the problem? This is happening across healthcare, so is this unique to radonc?
-Is it that residents are graduating and they are not getting a job after years of school, training, and debt? What is the best data for this to graduates truly not having any open positions to apply to. I say this as right now in Northeast Ohio alone I know of one group using a locums looking to hire a permanent doc, another using 3 locums trying to find 2-3 permanent positions, and another using 2 locums that needs 3 permanent docs. These are all centers not part of my institution. I have hired 8 physicians in 12 months and am recruiting 6 more. So is it that there are in fact jobs, but they are not the types of jobs people want (community vs main or solo vs multi-provider practice or academic vs non-academic or salary level or research or city vs rural or middle america vs coasts)? Totally understand not everyone wants to move to some of these centers in the rural midwest, or the environment is not what they want, but they are jobs. This difference matters in order to address the issue. Or is it number of jobs and the types of jobs? Is it a mismatch in we have tried to attract hyper academic, many MD/PhDs, to a market that supports having very few of them and so there is a mismatch of applicants wants and job availability? If we recruited mainly people who wanted to be community radoncs across the country would we have the same discussions?
-Is it the expansion of medschools/slots and residency programs/slots and this goes back to is there truly an oversupply and not enough demand? Or the demand is there does not match the interests of the applicants (ie tons of people graduating in Cali and NYC but jobs are needed in middle america)?
-Is it a DEI issue (or at least in part)? Our applicant pool is dominated by non-URM males so we are missing out on hundreds (or thousands) of women and URM that are applying to derm, radiology, etc. While this should absolutely be addressed and likely a contributing factor, it doesnt appear that the diversity in radonc is rapidly declining to explain the sudden change from when I applied to radonc in 2010 and by 3 years after I graduated in 2018 applicant numbers seemed to be dropping. If anything I thought I saw in recent papers some improvements in some components of diversity (at least gender) in radonc faculty.
-Is it a generational (I am a millennial technically too) or a manifestation of social media in that issues can now be brought out into the light to mass audiences more easily? I hope this audience can appreciate at times there has been disrespectful and unproductive comments on SDN, twitter, etc, often highly personal, about how bad they believe radonc is and people should run from it....that of course would impact potentially interested people in radonc. Perhaps this is the goal of these people, to sound the alarm to whatever the problem is and help these individuals go into another field. However, data will show that most other providers in medicine work longer hours for less pay and debatable have less impact as curing or palliating cancer...I realize many may disagree but I can tell you that I as Chair talk with many other Chairs whose faculty make far less and work more. However, I would think the generational and social media impact would impact all specialties fairly equally. So what appears unique to radonc? Or is this unique to radonc?
-Is it declines in private/community practice compensation with healthcare consolidation? In most academic university centers salaries have gone up (they were in the low $200k at U of M for new grads 10+ years ago and now are >$300k...I realize inflation is brutal recently but salaries went up). However, the days of private groups owning their equipment and getting the tech revenue is uncommon now, so the >$1m salaries (more than even almost every single Chair makes in the country based on SCAROP data) are hard to come by. However, salaries have tanked in dermatology (my wife is one and our family friend who just retired at 70yo from derm cleared $1m a year easily much of his career and now most derms (not all) make $250-400k...same major declines in general surgery, radiology, etc. So is this unique to radonc?
These are just some examples, but I would genuinely appreciate people who often write passionately about the decline of our field on this forum, and what the core problem is. Of course it is multi-factorial the cause, but what is the problem. This should be able to be clear and concise. Again, the causes and effects will be complex, but how would you state what the problem is in 1 short sentence.
I realize I am entering the lions den and I have read many of the incredibly negative and frankly disrespectful threads about me or my friends on SDN from people that have minimal to no personal knowledge or context to the things they write about. Not sure peoples motives for personal attack or how I have wronged them in my short career as faculty (~6.5 years)....but my name is Daniel so I hope my mom and dad were right giving me that name as the den has been entered!
If you would like for your anonymous voices to potentially be heard by the academic chairs across the country in Washington DC, let it rip.
Thanks
Dan