- Joined
- May 20, 2017
- Messages
- 74
- Reaction score
- 67
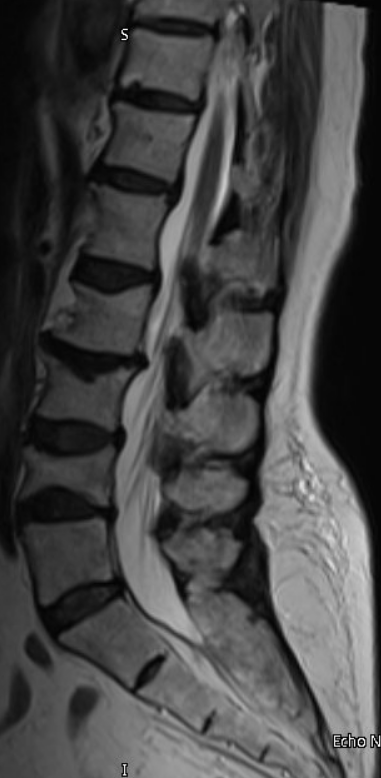
I have an 80 year old woman with osteoporosis and prior compression fractures. She developed significant acute axial low back pain February 18th without any inciting event. This was so severe that it resulted in a short hospitalization for pain control. Workup was negative except for chronic L3 and L4 compression fractures (I have included sagittal STIR and T2 lumbar spine MRI images below from 2/19/2023). Patient was referred to me in March. Pain was facetogenic on examination. I ended up performing bilateral L3-4 and L4-5 MBBs x2 followed by bilateral L3-4 and L4-5 RFA on 5/2/2023 and she had >90% relief for 2 weeks after the RFA. Unfortunately, 2 weeks later, she developed a sudden increase of axial pain symptoms without injury or inciting event. Repeat MRI lumbar of the lumbar spine was completed 6/9/2023 and showed acute L4 compression fracture with edema throughout the L5 vertebral body and increased signal in the L4-5 disc as well. I have attached sagittal MRI images below (STIR and T2).
Per the radiology report:
"1. Moderate acute diffuse L4 compression fracture without retropulsion.
2. Diffuse marrow edema in the L5 vertebral body without loss of vertebral body stature. This could be due to acute bone contusion without loss of vertebral body stature, however, this unexpected finding raises the possibility of infection or neoplasm, rather than trauma, as the etiology for the L4 and L5 abnormalities. Please correlate clinically. If the patient is going to have L4 kyphoplasty, it may be prudent to send the L4 core specimen for culture and cytology."
Patient had yearly CBC, BMP drawn 6/8/2023 with PCP which were completely normal except some thrombocytosis with platelets of 494.
I sent patient for ESR and CRP today.
CRP <4 (normal). ESR was elevated at 41 (normal range 0-30).
Patient has no systemic signs/symptoms of infection and her only complaint is low back pain. She does report a 12-13 pound weight loss since this pain started in February because “food just doesn’t taste good anymore”.
What would you recommend at this point?
I am tentatively planning L4 kyphoplasty and likely L5 at the same time as there is edema throughout the L5 vertebral body and if I fix L4 it seems probable to me that L5 could easily fracture in the acute postoperative period. I plan to take a biopsy of both levels and send for pathology/cytology and culture to rule out infection or neoplasm. Anything I am missing here? Should this be more urgently sent to ER/hospital for possibility of osteomyelitis? Any other subspecialty you would consult prior to kypho? Any labs I am missing? Thanks in advance for any advice.


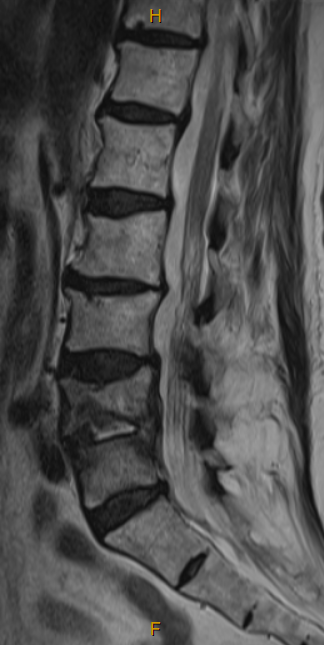
Per the radiology report:
"1. Moderate acute diffuse L4 compression fracture without retropulsion.
2. Diffuse marrow edema in the L5 vertebral body without loss of vertebral body stature. This could be due to acute bone contusion without loss of vertebral body stature, however, this unexpected finding raises the possibility of infection or neoplasm, rather than trauma, as the etiology for the L4 and L5 abnormalities. Please correlate clinically. If the patient is going to have L4 kyphoplasty, it may be prudent to send the L4 core specimen for culture and cytology."
Patient had yearly CBC, BMP drawn 6/8/2023 with PCP which were completely normal except some thrombocytosis with platelets of 494.
I sent patient for ESR and CRP today.
CRP <4 (normal). ESR was elevated at 41 (normal range 0-30).
Patient has no systemic signs/symptoms of infection and her only complaint is low back pain. She does report a 12-13 pound weight loss since this pain started in February because “food just doesn’t taste good anymore”.
What would you recommend at this point?
I am tentatively planning L4 kyphoplasty and likely L5 at the same time as there is edema throughout the L5 vertebral body and if I fix L4 it seems probable to me that L5 could easily fracture in the acute postoperative period. I plan to take a biopsy of both levels and send for pathology/cytology and culture to rule out infection or neoplasm. Anything I am missing here? Should this be more urgently sent to ER/hospital for possibility of osteomyelitis? Any other subspecialty you would consult prior to kypho? Any labs I am missing? Thanks in advance for any advice.
