- Joined
- Oct 13, 2010
- Messages
- 11,020
- Reaction score
- 169
Not really a clue what's happening at LLUMC... but, this is tragic.
LLUMC is supposed to be a very balanced residency program lifestyle-wise. Not sure why the rash of suicide there.
Very sad. This is tragic. Real depression. Judging by her picture. She’s skinny.
On a lighter note. I think way too many people are prescribed anti depressants. Many fat people who eat too much. The dsm criteria of depression has changed since the 1980s. Dsm 2? In the 1980s includes WEIGHT LOSS as part of depression.
Yet many people who write the dsm are brought out by drug manufacturers. So as Americans get fatter and fatter. The drug manufacturers bribed these dsm to include WEIGHT GAIN AS A PART OF DEPRESSION.
I know I’m going off topic slightly. But the vast majority of people who have true clinical depression are SKINNY. too many fat people are over prescribed anti depression drugs. They aren’t truly depressed.
The 3 people I know who have committed suicide (no drug overdose either...true clinical depression) recently in anesthesia have all been skinny with true clinically depressed as it was originally written in dsm-2 including a former colleague last September.
I think there are plenty of people with legit depression who are heavy. The "old" debilitating depression where you were very seriously suicidal, not eating, unable to get out of bed depression, severe psychomotor slowing etc. is seen less and less. Likely this is due to people getting treated BEFORE they get to that point. Perhaps this woman was one of them, and while that "type"/severity is surely horrendous, I do not believe that dysthymia/persistent depressive disorder, or "anxious/neurotic depression" (whatever you want to call it) is a walk in the park for people. Many of those people will have little correlation of symptoms to body habitus.
Someone mentioned good books in another post. While not an anesthesiologist, Peter. G. Kramer MD wrote an excellent book (voluminous but excellent) called Ordinarily Well. Should be required reading for any resident in psych IMO.
Wtf!?!I have seen very few suicidal people who are fat.
Get it? If u are truly fat. U lose interest in thing u love the most. If u are fat. U love food. If you are depressed. U stop eating and LOSE weight.
But fake depressed people GAIN weight.
We are over drugged society just because the drug manufacturers bribe the doc’s and policy makers.
Let me make it clear. I’m talking true clinical depression.
I think many (fat) people who are diagnosed with depression have subclinical depression.
How many actors with true depression who commit suicide are fat? I’m not talking the accidental overdose either. Robin Williams lost a lot of weight prior to killing himself.
My former colleague who committed suicide last fall was frail thin even with 4 kids.
my very overweight friend of 20 years suicided last year after a decades long struggle with depression.Very sad. This is tragic. Real depression. Judging by her picture. She’s skinny.
On a lighter note. I think way too many people are prescribed anti depressants. Many fat people who eat too much. The dsm criteria of depression has changed since the 1980s. Dsm 2? In the 1980s includes WEIGHT LOSS as part of depression.
Yet many people who write the dsm are brought out by drug manufacturers. So as Americans get fatter and fatter. The drug manufacturers bribed these dsm to include WEIGHT GAIN AS A PART OF DEPRESSION.
I know I’m going off topic slightly. But the vast majority of people who have true clinical depression are SKINNY. too many fat people are over prescribed anti depression drugs. They aren’t truly depressed.
The 3 people I know who have committed suicide (no drug overdose either...true clinical depression) recently in anesthesia have all been skinny with true clinically depressed as it was originally written in dsm-2 including a former colleague last September.
my very overweight friend of 20 years suicided last year after a decades long struggle with depression.
i suggest we leave psychiatry to those who have a better understanding of it than we gain from a rotation as a med student
Depressed people often find different ways to cope. Some eat obsessively. Some exercise. Some shop. Some starve themselves. It’s a complex issue. To suggest fat people don’t have “real” depression doesn’t seem well-informed.I have seen very few suicidal people who are fat.
Get it? If u are truly fat. U lose interest in thing u love the most. If u are fat. U love food. If you are depressed. U stop eating and LOSE weight.
But fake depressed people GAIN weight.
We are over drugged society just because the drug manufacturers bribe the doc’s and policy makers.
Let me make it clear. I’m talking true clinical depression.
I think many (fat) people who are diagnosed with depression have subclinical depression.
How many actors with true depression who commit suicide are fat? I’m not talking the accidental overdose either. Robin Williams lost a lot of weight prior to killing himself.
My former colleague who committed suicide last fall was frail thin even with 4 kids.
I have seen very few suicidal people who are fat.
Get it? If u are truly fat. U lose interest in thing u love the most. If u are fat. U love food. If you are depressed. U stop eating and LOSE weight.
But fake depressed people GAIN weight.
We are over drugged society just because the drug manufacturers bribe the doc’s and policy makers.
Let me make it clear. I’m talking true clinical depression.
I think many (fat) people who are diagnosed with depression have subclinical depression.
How many actors with true depression who commit suicide are fat? I’m not talking the accidental overdose either. Robin Williams lost a lot of weight prior to killing himself.
My former colleague who committed suicide last fall was frail thin even with 4 kids.
This is a very narrow minded assessment. "Fake" depressed people? Come on man.
Read the dsm-2
Dude...be like Elsa and LET IT GO!So i reckon u believe fibromyalgia as a diagnosis than?
My point is “real” clinical depression is a very grey area.
It’s way over diagnosed.
My best guess is 90% plus of people who commute suicide are NOT FAT.
I’m only stirring the pot here cause the pic o the anesthesia resident who committed suicide shows she seems NOT FAT.
Same with nyc medical doctor resident who jump to her death last month from nyc roof top.
The vast majority of people who committed suicide who have real clinical depression who drive them to commit suicide are not fat. True or false? Depression equals hopelessness. Losing desire to eat. Weight loss. Read the dsm-2
Munching away on food ain’t real depression.
My point is half the guys who write the dsm are bribed by the drug manufacturers. Too much conflict of interest these days.I probably wouldn't suggest reading a text from 1968 as the definitive source today.
My point is half the guys who write the dsm are bribed by the drug manufacturers. Too much conflict of interest these days.
Do u really believe the cholorprep study when the company got fined millions and key researcher was paid handsomely?
This is just sad. Praying for the lives of those impacted by this.
While I agree that there is some personal onus with some of these cases, let's not pretend that there aren't systematic problems that need to be fixed.
Sent from my XT1710-02 using Tapatalk
So i reckon u believe fibromyalgia as a diagnosis than?
My point is “real” clinical depression is a very grey area.
It’s way over diagnosed.
My best guess is 90% plus of people who commute suicide are NOT FAT.
I’m only stirring the pot here cause the pic o the anesthesia resident who committed suicide shows she seems NOT FAT.
Same with nyc medical doctor resident who jump to her death last month from nyc roof top.
The vast majority of people who committed suicide who have real clinical depression who drive them to commit suicide are not fat. True or false? Depression equals hopelessness. Losing desire to eat. Weight loss. Read the dsm-2
Munching away on food ain’t real depression.
Not really a clue what's happening at LLUMC... but, this is tragic.
Not really a clue what's happening at LLUMC... but, this is tragic.
I know of the person, and it has nothing AT ALL to do with the residency or it's pressures.
Very tragic and we are all just shell shocked. She had accomplished a lot and was very hard working.
Do you mean 2 out of 3 residents are anesthesia residents? The post says only 3 residents total suicided there, with 2 being in anesthesia.. whos the 3rd anes resident?
How are you so certain? I'm never certain with these things since people tend to be secretive about it. You'll ask them if it's xyz and they'll say no, doing great, residency is amazing. Even if its not directly due to residency, i find it difficult to imagine that your job as a resident which takes up most of your time had NOTHING AT ALL to do with it. For example, you may be depressed because your parents got killed in a car accident broke, but b/c you are in residency, you are left with minimal time to grief over it, or seek professional help (how many psychiatrists are available between the hours of 7pm and 5am? or on weekends?)
I think studies demonstrated that a lot of suicides happen to colleagues you wouldn't expect it to happen to, and then everyone is shocked, but i guess it shows how well you truly knew the person?
I think we can all agree (even those of us in other specialties) that residency is very demanding. It can suck in a myriad of different ways.Three resident suicides are not coincidence. It's a trend. Residency had something to do with it despite what the system will want to tell you.
How are you so certain? I'm never certain with these things since people tend to be secretive about it. You'll ask them if it's xyz and they'll say no, doing great, residency is amazing. Even if its not directly due to residency, i find it difficult to imagine that your job as a resident which takes up most of your time had NOTHING AT ALL to do with it. For example, you may be depressed because your parents got killed in a car accident broke, but b/c you are in residency, you are left with minimal time to grief over it, or seek professional help (how many psychiatrists are available between the hours of 7pm and 5am? or on weekends?)
I think studies demonstrated that a lot of suicides happen to colleagues you wouldn't expect it to happen to, and then everyone is shocked, but i guess it shows how well you truly knew the person?
I think we can all agree (even those of us in other specialties) that residency is very demanding. It can suck in a myriad of different ways.
Some of those can be improved, some probably can't - or rather, can't without major changes like increasing residency length which very few people want.
In terms of work hours, in residency to achieve better hours that you'd most likely have to make residency longer. That's certainly an option, and now that I'm through with training I would have no objection to that. Everyone might not agree to that though. There is also much to be said about patient continuity of longer shifts. That's obviously more the case for some specialties than others of course - take a look at the trial the surgeons did a few years back looking at this very issue.There is a difference between a demanding job and the toxic culture that exists within medicine. We are constantly hearing stories of resident suicides and physician burnout. I remember my first day of medical school the dean gave a speech saying we were entering a profession that had one of the highest rates of suicide, depression, substance abuse, and divorce. Why is that acceptable?
There is something rotten in our profession right now and it starts in medical school and continues into retirement. Until we acknowledge it and stop with the culture that encourages you to brag how many hours straight you can work without sleep, more lives will be ruined.
We must hold the system accountable and not allow them to shift the blame back to us. The lectures and powerpoints on how to recognize and cope with sleep deprivation and burnout are not only insulting, but they only serve to give the institutions responsible a pass. I remember sitting through a PowerPoint presentation about recognizing the signs of sleep deprivation during my intern year. When the lecture finished I asked why don't we create a system where sleep deprivation is not an issue. The response I got was basically a chuckle. With the incessant discussion and studies about resident work hour limits, the only outcomes ever mentioned are patient morbidity and mortality. The physicians' physical, mental, and emotional well-being isn't even given a glancing mention. I have a problem with that.
You are making a lot of assumptions. Her work and the residency could just as well have been the best part of her life and a respite from her other problems. I don’t know, but unless you know, don’t assume. Especially if you are not close to the situation, it’s all conjecture.
In terms of work hours, in residency to achieve better hours that you'd most likely have to make residency longer. That's certainly an option, and now that I'm through with training I would have no objection to that. Everyone might not agree to that though. There is also much to be said about patient continuity of longer shifts. That's obviously more the case for some specialties than others of course - take a look at the trial the surgeons did a few years back looking at this very issue.
Burnout in attendings, at least in my specialty, has very little to do with medicine itself and more everything associated with it - increasing paperwork, loss of autonomy, assembly line practice, and so on. This has nothing to do with a toxic medical culture and much more to do with increasing administration.
Meanwhile, nurses are shift workers from the start. They know their hours and they know exactly where they stand in terms of value. If they work extra, they demand extra pay. As doctors we are taught to "stay until the work is done." Is it a coincidence that nurses don't experience burnout to the same degree as physicians? I think not.
I disagree; mainly because plenty of doctors are shift workers. As someone who is perpetually on the verge of burnout, I see it as more a matter of loss of autonomy or a mismatch between expectations/reality.
When I was in training, the thing that weighed on me most, and at times pushed me in the general direction of burnout, wasn't the long hours, the sleep deprivation, or taking another human's life into my hands several times per day.
It was being a grown up adult, a married man, a father, a person who made the cut to get into medical school and graduated and passed the USMLE, a person who held an unrestricted license to practice medicine ... and yet I lived and worked in this surreal kindergarten-like world where I and a bunch of other people like me were constantly seeking approval from attendings like they were distantly neglectful parents.
I don't remember having that kind of relationship with my professors in college or medical school. There wasn't a culture that revolved around "staying off the radar" or pleasing anyone. In my interactions with them, I was a respected adult learner, and they were there to guide me. Somehow, when I became an intern, I became a child again. And to make it worse, to an extent I embraced that role because I understood it to be the only way I'd be able graduate and move on to a less caustic place in life.
I actually felt worse about it because I voluntarily assumed that role.
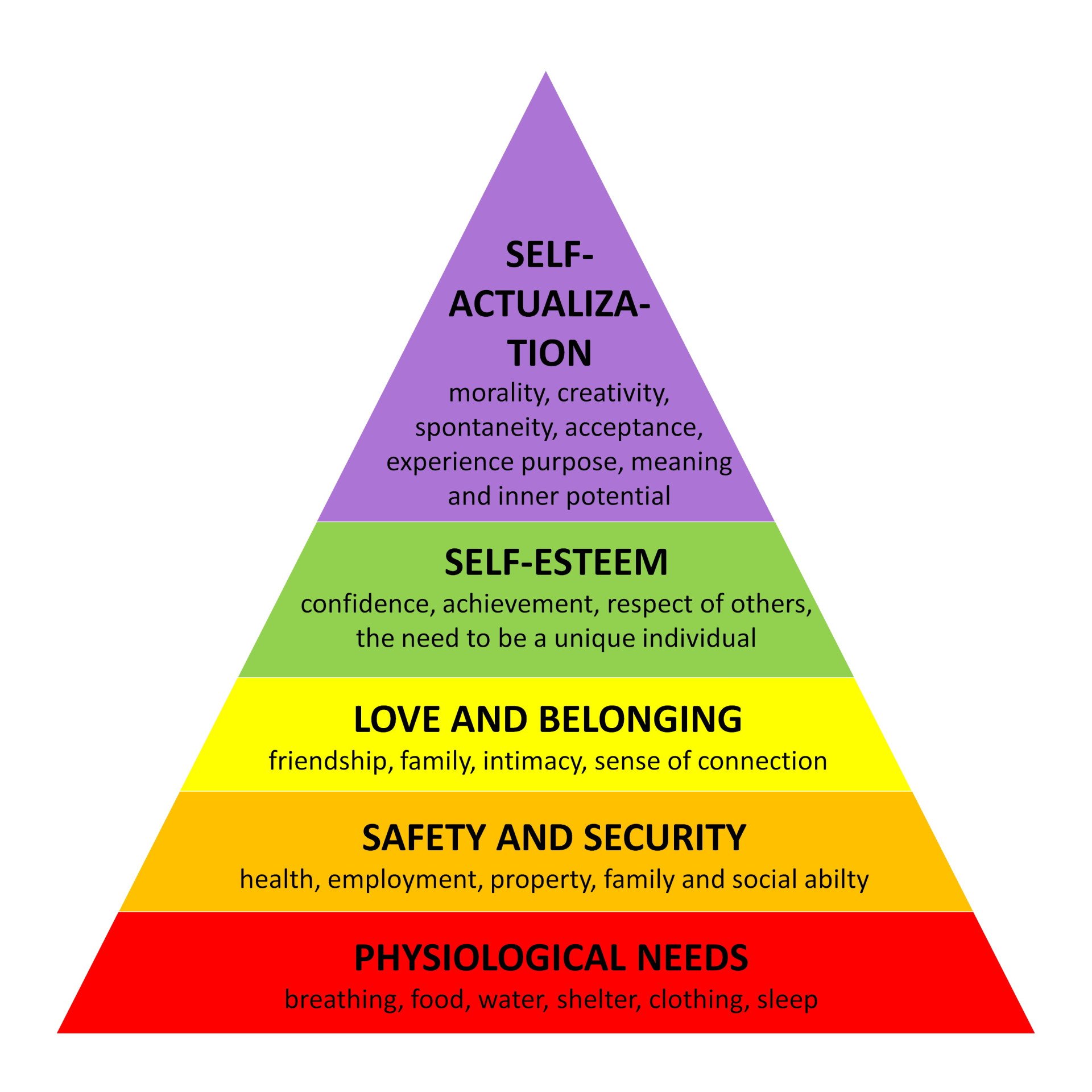
I'm just an armchair psychiatrist, but I can't help but think of of Maslow's hierarchy of needs. You've got a bunch of mature adult high achievers, fresh out of medical school, in that top self-actualization tier of the pyramid, and then they enter the world of GME and get roughly kicked down to a level where all of a sudden the overriding concerns are for "security, order, law, stability, freedom from fear" ... one bare notch above basic biological needs for food and shelter. Safety needs.
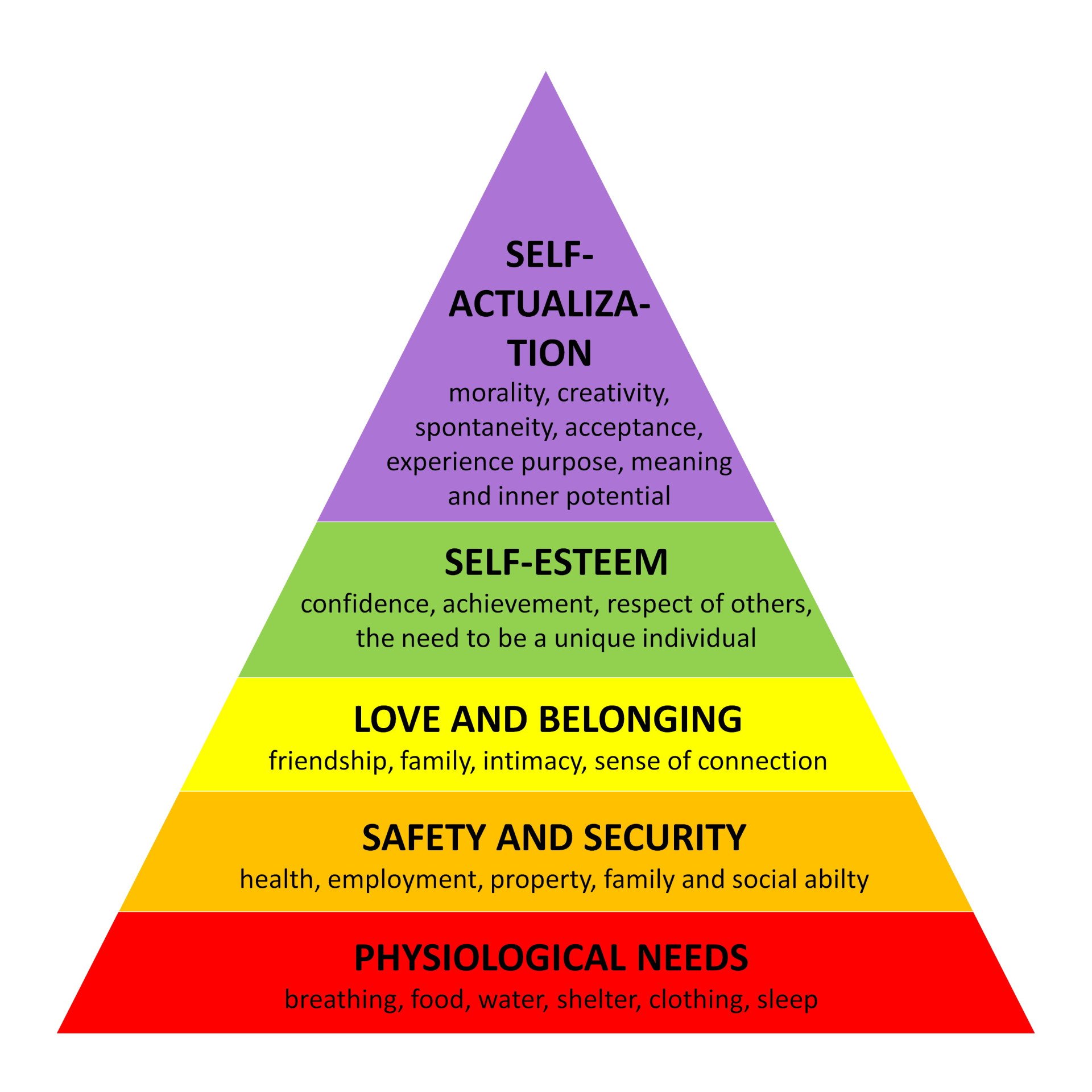
That stuff at the top of the pyramid is important, and while residency could and should be structured to lift people up, too often it feels like we've created some kind of gradeschool-esque popularity contest where the residents need to show a smile, never show a sign of fatigue, always verbalize enthusiasm about that high-value afternoon wound washout add-on case aka opportunity to excel even when we know they're just as disappointed in getting an extra couple hours of low-yield labor as we are.
Over and over again I've seen very junior trainees who are just as incompetent as their peers, but their demeanor, speech patterns, personality, sense of humor get them "on the radar".
A majority of staff eval narratives include comments on attitude. Even when complimentary, when residents see such comments, it just reinforces the notion that they're being judged on nonclinical personality trait intangibles.
There's something fundamentally pathological and humiliating about our system. It's no wonder that physician burnout, depression, and suicide are such problems. I think we fixate on work hours being the main culprit waaaaaay too much. We're the better part of two decades into this work hour limit experiment and residents are still burning out and killing themselves. It's not because they're tired.
I think it's because the system makes them feel small.
I disagree; mainly because plenty of doctors are shift workers. As someone who is perpetually on the verge of burnout, I see it as more a matter of loss of autonomy or a mismatch between expectations/reality.
Granted I didn't do an anesthesia residency, but there was very little in my training that seemed like just using me for cheap labor. I mean, on inpatient we rarely admitted more than 5-7 patients/24 hours. At most, that's 1 full time attending. To accomplish that we had a team of 3-4 interns and 2 upper levels. Hiring another physician would have been cheaper than all of us doing the work, and fairly inefficiently I would say. As for time spent not learning, I guess that depends how you look at it. At a certain point, I didn't really feel like writing daily progress notes on some of those same hospitalized patients was teaching me all that much but that's part of the job of being a doctor. And yeah some of the noon conference lectures weren't all that good, but not all CME is good either. You can't win everything. I dunno, maybe I was lucky but I don't recall, even at the time, thinking that much of residency was a waste of my time.Assuming an 80 hour work week, what percentage of those hours are dedicated towards actual medicine and learning? Residency doesn't have to be extended, but residents have to stop being used as cheap labor. We are opening up more doors for lesser trained people to do the same jobs as physicians at the same time we are advocating for lengthening of physician training? Something doesn't make sense here.
You are describing our medical system. That is the culture. Whether it is fellow docs or administrators responsible doesn't matter. There is something rotten that needs to be taken care of.
We like to discuss the physician vs. nurse dichotomy on this board and I think that gets to the root of some of the problem. We are indoctrinated early on to not ask for help, not show emotion, and always demonstrate a duty towards patients. The administrators turn that mindset against us. Meanwhile, nurses are shift workers from the start. They know their hours and they know exactly where they stand in terms of value. If they work extra, they demand extra pay. As doctors we are taught to "stay until the work is done." Is it a coincidence that nurses don't experience burnout to the same degree as physicians? I think not.
Granted I didn't do an anesthesia residency, but there was very little in my training that seemed like just using me for cheap labor. I mean, on inpatient we rarely admitted more than 5-7 patients/24 hours. At most, that's 1 full time attending. To accomplish that we had a team of 3-4 interns and 2 upper levels. Hiring another physician would have been cheaper than all of us doing the work, and fairly inefficiently I would say. As for time spent not learning, I guess that depends how you look at it. At a certain point, I didn't really feel like writing daily progress notes on some of those same hospitalized patients was teaching me all that much but that's part of the job of being a doctor. And yeah some of the noon conference lectures weren't all that good, but not all CME is good either. You can't win everything. I dunno, maybe I was lucky but I don't recall, even at the time, thinking that much of residency was a waste of my time.
See I don't consider administration stuff to be the culture of medicine. I consider that more like the stuff that PGG mentions a few posts up. If the administration stuff bothers you, find a job where that isn't an issue. I had a DPC clinic for a few years that had none of that burden. No insurance, no boss other than myself, just seeing patients all day, writing notes that contained what I thought was important not what Blue Cross did. I did have to run the business part, but that was maybe 1 hour/week of work.
As to nurses, they burn out too. In fact, a study from 7 years ago showed that hospital nurses who actually take care of patients have a burn out rate of around 35%. That's not as high as the roughly 50% rate of medicine as a whole, but its still a pretty high number.
As for "staying til the work is done" versus strict shift work... depends how you're paid. If you get paid based on the work you do, then you do get paid more for working more. If you're paid hourly, you also get paid more. If you're straight salary, you need a better contract. I did a year of urgent care a few years back. We were salary with an expectation of working X shifts/month with defined hours. After about 2 months I noticed that I stayed late probably 2/3rds of the time with last minute walk ins. So I went to admin and they adjusted my total shifts worked down by 1/month. Basically it worked out to them paying me for 13 hours/day despite the official hours being 8-8. If you're staying late and not getting paid, do the same.
I personally think internal medicine residency is too long as it is. I think the training could be completed in 2 years if we cut some of the fat out. I think anesthesia residency could be cut by a year as well. The idea that if we cut work hours then we would have to extend residency doesn't make much sense to me when we have midlevels doing our same jobs independently with less time training. That's a discussion for another thread, though.
@GravelRider, I totally agree that residency could and should be shortened, a year less seems about right. Unfortunately, the people who could change things are also the ones who benefit from keeping the cheap labor force around as long as possible.
