- Joined
- Sep 7, 2014
- Messages
- 3,221
- Reaction score
- 5,953
Was googling for more shorter courses of palliative spine RT and noticed this recent pub from the god of palliative spine rt:
 ro-journal.biomedcentral.com
I remember some recent posts on here where people said they were using 5x5 for palliative spine, or at least for cord compression. Is this becoming a common practice, and do you just use 5 fx sbrt constraints?
ro-journal.biomedcentral.com
I remember some recent posts on here where people said they were using 5x5 for palliative spine, or at least for cord compression. Is this becoming a common practice, and do you just use 5 fx sbrt constraints?
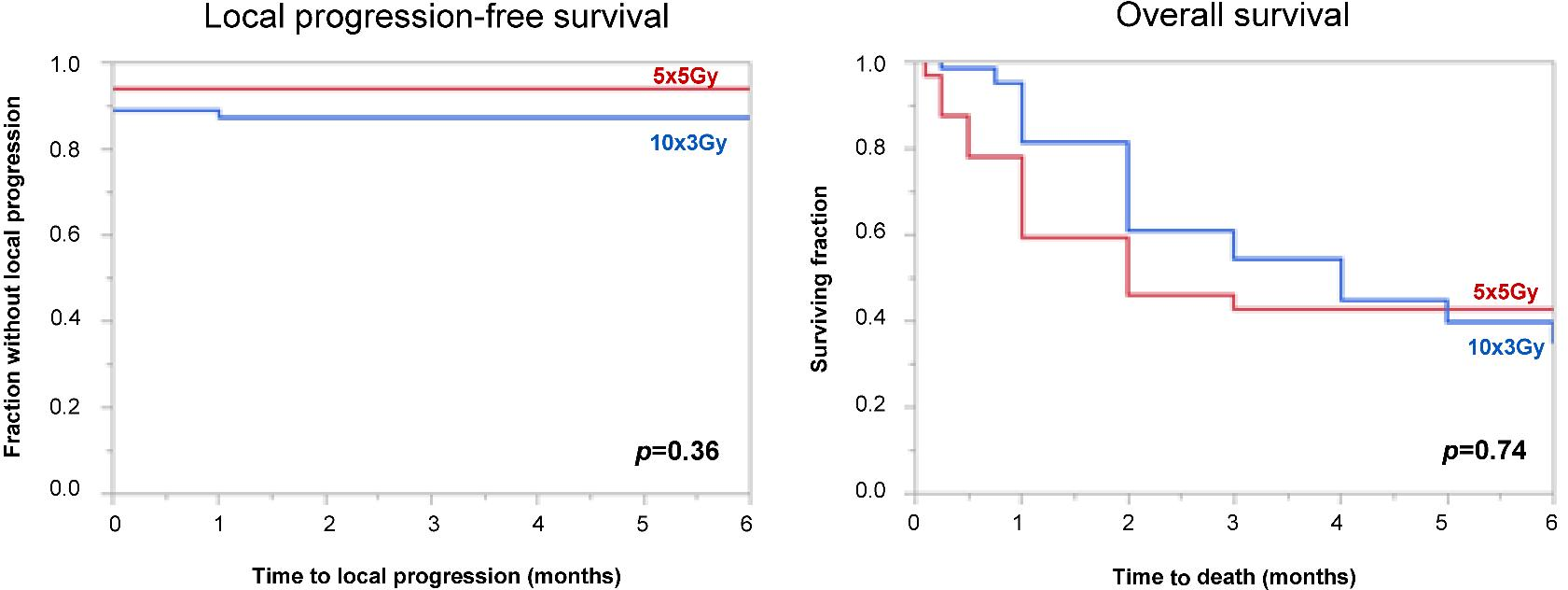
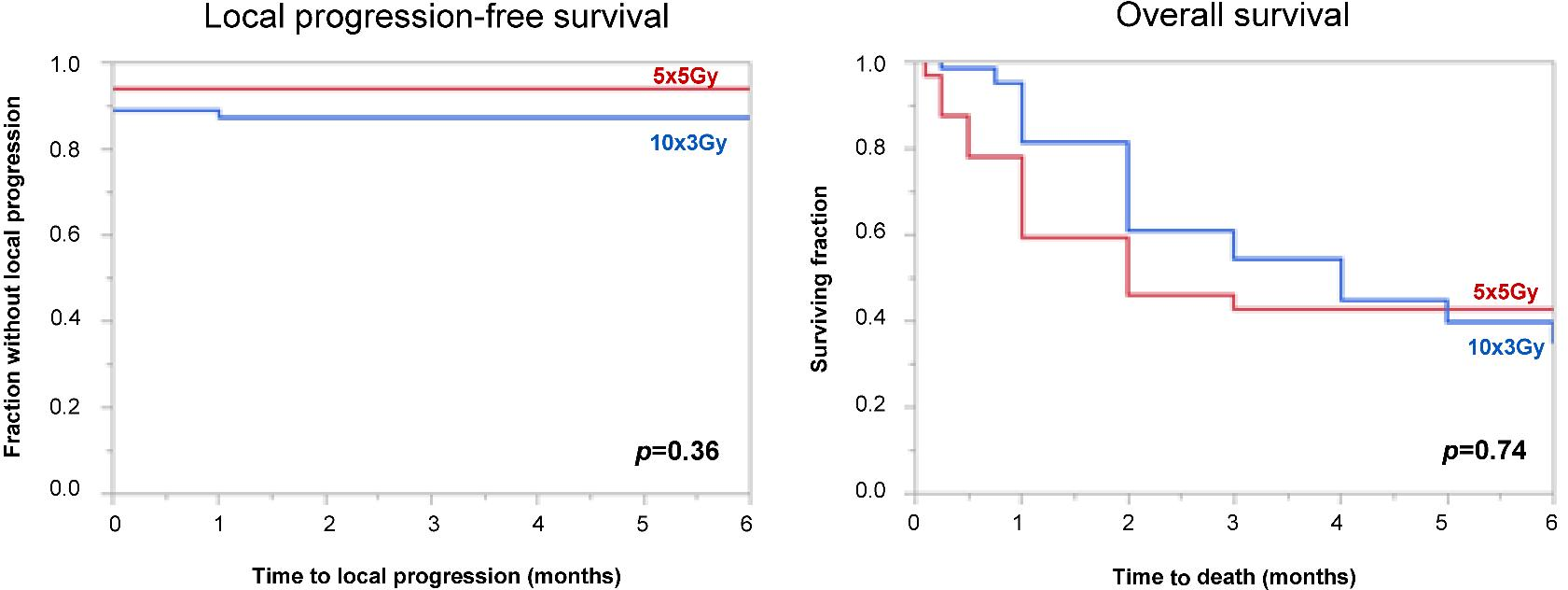
Comparison of 5 × 5 Gy and 10 × 3 Gy for metastatic spinal cord compression using data from three prospective trials - Radiation Oncology
Background In a palliative situation like metastatic spinal cord compression (MSCC), overall treatment time of radiotherapy should be as short as possible. This study compared 5 × 5 Gy in 1 week to 10 × 3 Gy in 2 weeks in a prospective cohort. Methods Forty patients receiving 5 × 5 Gy in a phase...