- Joined
- Jul 12, 2004
- Messages
- 5,289
- Reaction score
- 4,988
I've got an ID question, however it doesn't appear there is a specific ID subforum. So hopefully this forum is OK.
I treated a patient in the ED for a complicated UTI / early pyelonephritis. She ended up being stable, not septic, gave one dose of Rocephin IV and discharged her with antibiotics. cefadroxil 500 mg PO BID x7 days.
Her urine culture returned a few days later
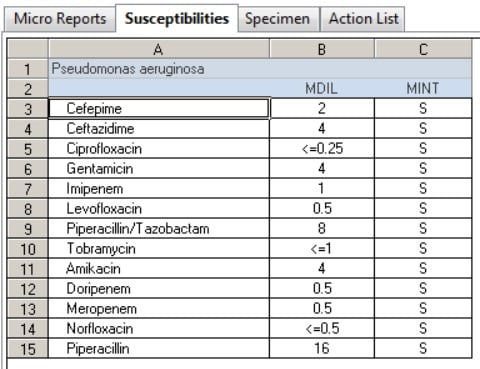
100,000 cfu/ml Pseudomonas aeruginosa
with pan-sensitivity
Think the cefadroxil will be OK? Or should she be changed to something else like a fluoroquinolone or cefpodoxime?
Thanks.
I treated a patient in the ED for a complicated UTI / early pyelonephritis. She ended up being stable, not septic, gave one dose of Rocephin IV and discharged her with antibiotics. cefadroxil 500 mg PO BID x7 days.
Her urine culture returned a few days later
100,000 cfu/ml Pseudomonas aeruginosa
with pan-sensitivity
Think the cefadroxil will be OK? Or should she be changed to something else like a fluoroquinolone or cefpodoxime?
Thanks.

