- Joined
- May 30, 2005
- Messages
- 23,342
- Reaction score
- 14,993
Amniofix CPT during intra-op use? RVU 2.45 in facility, 4.29 non-facility
This is how you Ballers get your 10K?
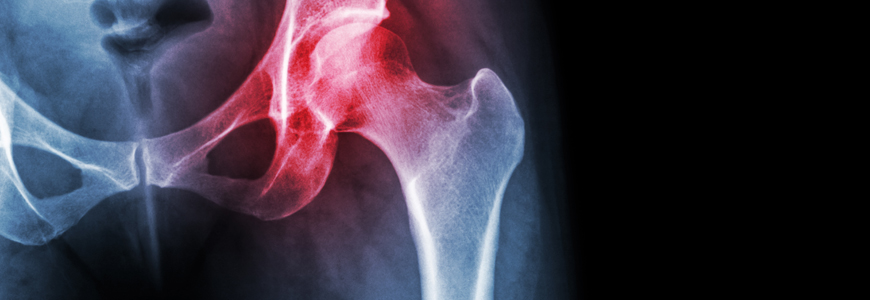
Comparative Effect between Infiltration of Platelet-rich Plasma and the Use of Corticosteroids in the Treatment of Knee Osteoarthritis: A Prospective and Randomized Clinical Trial
Marianna Ribeiro de Menezes Freire 1, Philippe Mota Coutinho da Silva 1, Arthur Rangel Azevedo 2, Denison Santos Silva 3, Ronald Bispo Barreto da Silva 3, Juliana Cordeiro Cardoso 3
Affiliations expand
PMID: 33093718 PMCID: PMC7575359 DOI: 10.1016/j.rbo.2018.01.001
Abstract
Objectives This study aimed to analyze the efficacy of platelet-rich plasma obtained from the peripheral, autologous blood of the patients in pain complaints reduction and functional improvement of knee osteoarthritis compared with the standard treatment with injectable corticosteroid, such as triamcinolone. Methods The patients were followed-up clinically at the preinfiltrative visit, with quantitative evaluation using the Knee Society Score (KSS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, and the Kellgren and Lawrence scales. In addition, they were reevaluated with the same scales after 1 month and 6 months of intervention with 2.5 mL of triamcinolone acetate or 5 mL of platelet-rich plasma. The study was performed on 50 patients with knee osteoarthritis treated at the Medical Specialty Center and randomly divided into equivalent samples for each therapy. Results The present study verified the reduction of pain scores, such as the WOMAC score, and elevations of functional scales, such as the KSS, evidenced in 180 days when using platelet-rich plasma, a therapy that uses the autologous blood of the patient and has fewer side effects. Conclusion Although both platelet-rich plasma and corticosteroid therapies have been shown to be effective in the reduction pain complaints and functional recovery, there was a statistically significant difference between them at 180 days. According to the results obtained, platelet-rich plasma presented longer-lasting effects within 180 days in the treatment of knee osteoarthritis.
Keywords: corticosteroids; osteoarthritis; platelet-rich plasma.
The Author(s). This is an open access article published by Thieme
Arthroscopy
. 2020 Oct 19;S0749-8063(20)30843-4. doi: 10.1016/j.arthro.2020.10.013. Online ahead of print.
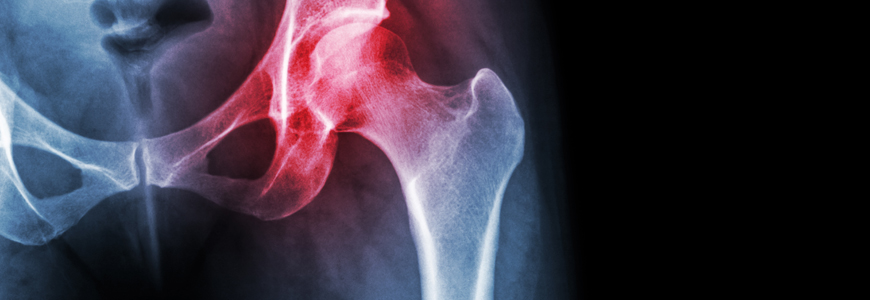
Intra-articular platelet-rich plasma combined with hyaluronic acid injection for knee osteoarthritis is superior to PRP or HA alone in inhibiting inflammation and improving pain and function
Zhe Xu 1, Zhixu He 2, Liping Shu 3, Xuanze Li 4, Minxian Ma 3, Chuan Ye 5
Affiliations expand
PMID: 33091549 DOI: 10.1016/j.arthro.2020.10.013
Abstract
Purpose: The goal of this study was to evaluate the effectiveness and explore the therapeutic mechanisms of PRP combined with HA as a treatment for knee osteoarthritis (KOA).
Methods: In total, 122 knees were randomly divided into HA (34 knees), PRP (40 knees), and PRP+HA (48 knees) groups. Platelet densities in whole blood and PRP were examined using Wright-Giemsa staining. Visual Analogue Scale (VAS), Lequesne, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Lysholm scores and postoperative complications were evaluated. High-frequency color Doppler imaging was used to observe the synovium and cartilage. Enzyme-linked immunosorbent assays (ELISAs) were used to quantify interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), matrix metalloproteinase-3 (MMP-3), and tissue inhibitor of metalloproteinase-1 (TIMP-1) levels in synovial fluid.
Results: The platelet density in PRP was 5.13-times that in whole blood (P = .002). At 24 months, pain and function scores in the PRP+HA group were better than those in the HA and PRP alone groups (Ppain = .000; Pfunction = .000). At 6 and 12 months, synovial hyperplasia in the PRP and PRP+HA groups was improved (P < .05). After 6 and 12 months, the synovial peak systolic velocity (PSV), synovial end diastolic velocity (EDV), systolic/diastolic ratio (S/D) and resistance index (RI) were improved in the PRP+HA group (P < .05). Complications were highest in the PRP group (P = .008). After 6 and 12 months, IL-1β, TNF-α, MMP-3, and TIMP-1 in the PRP and PRP+HA groups decreased (P < .05), with more apparent inhibition in the PRP+HA group (P < .05).
Conclusions: PRP combined with HA is more effective than PRP or HA alone at inhibiting synovial inflammation and can effectively improve pain and function and reduce adverse reactions. Its mechanism involves changes in the synovium and cytokine content.
Copyright © 2020. Published by Elsevier Inc.
Humans Have Salamander-Like Ability to Regrow Cartilage in Joints
Regeneration offers possible osteoarthritis treatmentphysicians.dukehealth.org
Are there cost-effective ways to offer PRP injections to patients? My understanding is that it is all out of pocket for them. What is the typical cash price for in office vs ASC procedures?
Along these lines - what r typical charges?Are there cost-effective ways to offer PRP injections to patients? My understanding is that it is all out of pocket for them. What is the typical cash price for in office vs ASC procedures?
500-1500...i usually charge 800....i charge 500 for established patients.....all done with fluoro and/or US, not blind
That is incredibly cheap. Likely due to competition. Many pain and ortho offering in LA, but much higher prices. Average was $1200. I was the one of the cheaper ones at $900$350-500 in my area. Must be 75 practices in 20 mile radius performing. Really no way to pencil it out if using a mfr kit and need to spin yourself.
$300 for a MRI. That's a great price...Maybe I’m being a little cheap. 500-750 all over town. 350 for current patients in some aggressive practices. Can get MRIs for under 300 cash pay locally for reference.
there are several big names that charge more- regennex, steadman etc but they are pulling patients from out of state
Competition in action. I have patients everyday that it’s cheaper to pay out of pocket then deductible for imaging.$300 for a MRI. That's a great price...
Competition in action. I have patients everyday that it’s cheaper to pay out of pocket then deductible for imaging.
maybe we should be careful what we wish for... sos makes me seem inexpensive option
Network wants to charge patients $250 for PRP and give us 1.79 wRVUs
does any insurance company pay for this?Network wants to charge patients $250 for PRP and give us 1.79 wRVUs
does any insurance company pay for this?
Im employed, have to charge $1200 for PRP due to the blood draw placing me in the regulatory classification of a blood bank and the need for a Clia license, which I dont have in my office so I do it at the mothership’s radiology suite with lab staff. The one good thing is that that lab testing verifies that we get nearly a million platelets.
I hate that price though, and talk most people out of it. I dont think it should be more than $300-400. I had excellent results in a rectus abdominus tear that I likely did for free since by some miracle comp agreed to pay a lowball fee
But that is only two fools you have to dupe to recoup the costs.I looked at the Regenex course for joint injections...$6,800 to get trained 😵
I looked at the Regenex course for joint injections...$6,800 to get trained 😵
The Ritz-Carlton nightly rates and room service Dom Perignon are not cheapI looked at the Regenex course for joint injections...$6,800 to get trained 😵
On that note, does anyone have a good diagnostic ultrasound course/book/certification they can recommend?the little structures may not all need to be hit, but they need to be on the differential.
attributing all knee pain with degenerative changes to OA alone and flooding the joint space with injectate is a bit like calling all back pain DDD and performing an epidural.
your differential is only as good as your knowledge of the anatomy and pathophysiology... find a good anatomical atlas and you will realize how many structures there are you have NEVER heard about.
high quality MSK work makes doing the same B/B spine procedures look like a box of crayons in the rec room.
true.....but he needs to walk before he runs. Then build on the foundation. I have some basic adipose and BMAC videos if you email me.the little structures may not all need to be hit, but they need to be on the differential.
attributing all knee pain with degenerative changes to OA alone and flooding the joint space with injectate is a bit like calling all back pain DDD and performing an epidural.
your differential is only as good as your knowledge of the anatomy and pathophysiology... find a good anatomical atlas and you will realize how many structures there are you have NEVER heard about.
high quality MSK work makes doing the same B/B spine procedures look like a box of crayons in the rec room.
Learning pattern recognition for Injections isn’t too tough. Diagnostic Msk US going to take those 10k hours... but you see a normal enough times pathology pokes you in the eyeOn that note, does anyone have a good diagnostic ultrasound course/book/certification they can recommend?
Bianchi and martinoli book is the Bible of diagnostic Msk US. About 600 pages. $500 tooLearning pattern recognition for Injections isn’t too tough. Diagnostic Msk US going to take those 10k hours... but you see a normal enough times pathology pokes you in the eye
Bianchi and martinoli book is the Bible of diagnostic Msk US. About 600 pages. $500 too
consider buying Jacobson for $50
I may have found a pdf of it once when I google searched it....Unless you get the trade paperback “international” version but that would be immoral and illegal and I would never suggest that you do that.
I mean I heard of someone who found it on google. Amazing what you can find on the www!I may have found a pdf of it once when I google searched it....
Unfortunately this is true and it is a steep learning curve.high quality MSK work makes doing the same B/B spine procedures look like a box of crayons in the rec room.
Bianchi and martinoli book is the Bible of diagnostic Msk US. About 600 pages. $500 too
consider buying Jacobson for $50
Many people lose faith and leave the church.They used to be a Regenexx affiliate??
Many people lose faith and leave the church.
Franchise fees and secret marketing sauce not always worth the squeeze.
If kits still cost about $200 I’m not interested. I’ve been “kit-less” for almost 10 years.
Are you able to produce the same quality “product” without a kit? Is the kit merely to make the process easier and quicker?
