What diagnosis did u use them for in chronic pain?
Send to
Scand J Pain. 2017 Oct;17:325-329. doi: 10.1016/j.sjpain.2017.08.013. Epub 2017 Sep 12.
Erector spinae plane (ESP) block in the management of post thoracotomy pain syndrome: A case series.
Forero M1,
Rajarathinam M2,
Adhikary S3,
Chin KJ4.
Author information
Abstract
BACKGROUND AND AIMS:
Post thoracotomy pain syndrome (PTPS) remains a common complication of thoracic surgery with significant impact on patients' quality of life. Management usually involves a multidisciplinary approach that includes oral and topical analgesics, performing appropriate interventional techniques, and coordinating additional care such as physiotherapy, psychotherapy and rehabilitation. A variety of interventional procedures have been described to treat PTPS that is inadequately managed with systemic or topical analgesics. Most of these procedures are technically complex and are associated with risks and complications due to the proximity of the targets to neuraxial structures and pleura. The ultrasound-guided erector spinae plane (ESP) block is a novel technique for thoracic analgesia that promises to be a relatively simple and safe alternative to more complex and invasive techniques of neural blockade. We have explored the application of the ESP block in the management of PTPS and report our preliminary experience to illustrate its therapeutic potential.
METHODS:
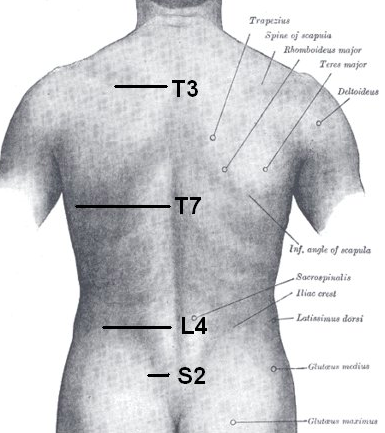
The ESP block was performed in a pain clinic setting in a cohort of 7 patients with PTPS following thoracic surgery with lobectomy or pneumonectomy for lung cancer. The blocks were performed with ultrasound guidance by injecting 20-30mL of ropivacaine, with or without steroid, into a fascial plane between the deep surface of erector spinae muscle and the transverse processes of the thoracic vertebrae. This paraspinal tissue plane is distant from the pleura and the neuraxis, thus minimizing the risk of complications associated with injury to these structures. The patients were followed up by telephone one week after each block and reviewed in the clinic 4-6 weeks later to evaluate the analgesic response as well as the need for further injections and modification to the overall analgesic plan.
RESULTS:
All the patients had excellent immediate pain relief following each ESP block, and 4 out of the 7 patients experienced prolonged analgesic benefit lasting 2 weeks or more. The ESP blocks were combined with optimization of multimodal analgesia, resulting in significant improvement in the pain experience in all patients. No complications related to the blocks were seen.
CONCLUSION:
The results observed in this case series indicate that the ESP block may be a valuable therapeutic option in the management of PTPS. Its immediate analgesic efficacy provides patients with temporary symptomatic relief while other aspects of chronic pain management are optimized, and it may also often confer prolonged analgesia.
IMPLICATIONS:
The relative simplicity and safety of the ESP block offer advantages over other interventional procedures for thoracic pain; there are few contraindications, the risk of serious complications (apart from local anesthetic systemic toxicity) is minimal, and it can be performed in an outpatient clinic setting. This, combined with the immediate and profound analgesia that follows the block, makes it an attractive option in the management of intractable chronic thoracic pain. The ESP block may also be applied to management of acute pain management following thoracotomy or thoracic trauma (e.g. rib fractures), with similar analgesic benefits expected. Further studies to validate our observations are warranted.