- Joined
- Jan 6, 2021
- Messages
- 36
- Reaction score
- 330
Metastatic Disease as a Distinct Discipline in Radiation Oncology
This Viewpoint discusses the advantages of having a dedicated metastatic disease radiation oncology program addressing the specific needs of patients with metastatic cancer.
Based on the one of the last rad onc-related surveys (of which there are 494 per year) published by ASTRO, a primary concern of rad oncs was wanting to be seen as an oncologist rather than just a rad onc (aka being a technician/button pusher). Almost everyone wanted to be seen as an oncologist but very few felt that their practice reflected that desire.
Then we get this hot garbage published as a viewpoint in JAMA Onc from 3 attendings in the new rad onc specialty called PROMISE (not even making this up) at MSKCC that metastatic disease needs to be a distinct specialty in rad onc. The reasons they give essentially boils down to "stage IV patients are complicated and primary disease site rad oncs can't handle the complexity." I wanted to translate that for the rest of us:
"We are in academics and need to justify our existence. We somehow need to be able to ask for more funding for our 'new 'disease site. Most importantly, we would like to be considered for professorships and leadership positions and to do that, we need a 'disease site' and since one wasn't open when we took a job at MSKCC, we created our own and want to try to try and enforce this new model on other rad oncs across the country. In addition, MSKCC is on a non-RVU model so this is possible because we all know if this were Pitt or another RVU-based academic practice, this would never happen as the other rad oncs would never refer their patients and RVUs to us. #iamarealdoctor #radoncrocks"
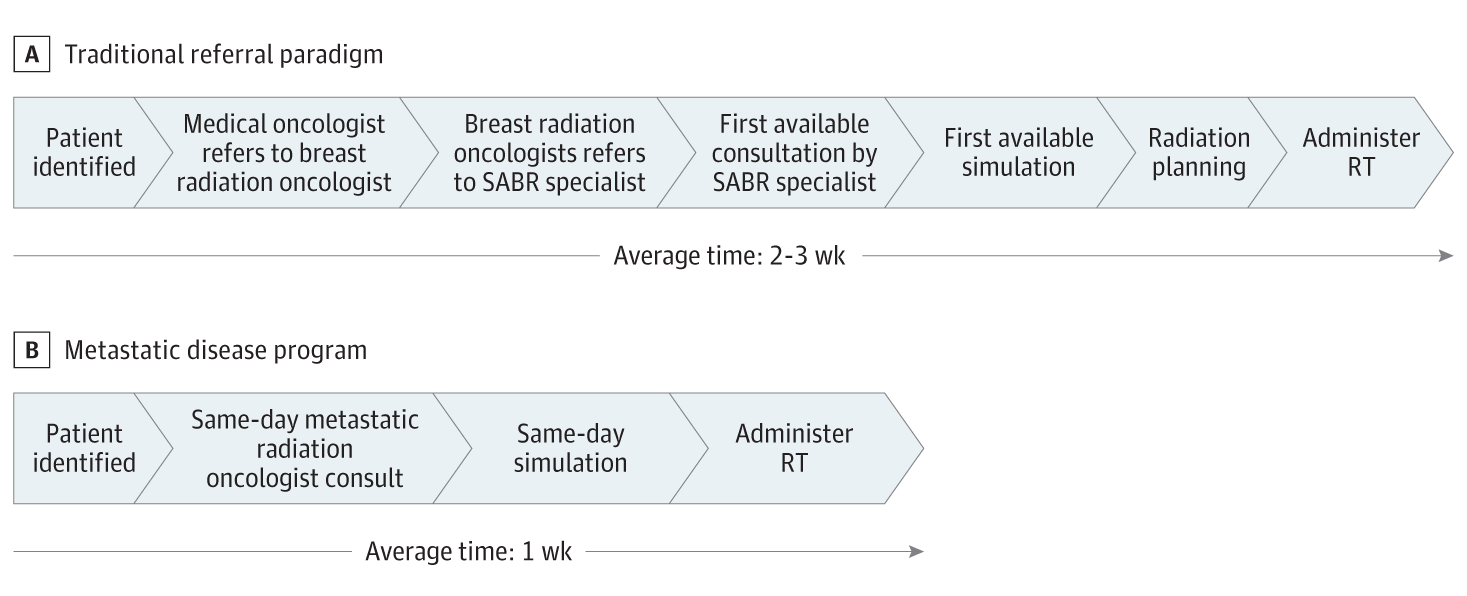
Someone please tell me I am overreacting but this viewpoint is as bad as my idea of shaming medical students who match at terrible programs - hot garbage that we will all be dumber for having read. So a breast rad onc can't SBRT a right hip met? They have a hilarious figure in the paper that shows how the traditional referral paradigm is 2-3 weeks. Because we all know we can't sim and treat an urgent palliative patient unless they are treated by a rad onc who specializes in metastatic disease. So now the patient has two rad oncs? One who treated the primary breast cancer and then another rad onc who just does the SABR/SBRT? Just writing that was painful. The fact that this was accepted by JAMA Onc is a joke.
Are there really academic rad oncs that just do SABR/SBRT? I know it is a thing but how is it really a thing we are publishing about? We should be trying to hide that embarrassing fact from everyone. I'm just imagining what it must be like to be a button pushing basement catfish who doesn't treat their own patients and is just referred stage IV patients to essentially "spot-weld" random mets throughout the body. I'm embarrassed for any rad onc who does that. This is the type of "research" that is killing our field. But hey, as long as you get promoted based on a pile of retrospective chart reviews and JAMA Onc viewpoints, it's all good
To the PROMISE attendings of MSKCC, thank you for advocating for us to become less of oncologists and have less ownership of patients. You are shining paragons of our field and we all cannot wait to give up ownership of our patients and be seen even more as technicians by our referring med oncs and surgeons.
We should be advocating that primary disease site attendings are up to date on the latest treatment techniques so patients can be treated by their ONCOLOGIST who can SRS a brain met and SABR/SBRT a right hip met after they treated the breast primary. That's how you become an ONCOLOGIST to the patient and to the med onc or surgeon. You do not refer to another rad onc just to do SABR/SBRT - it makes both rad oncs look like button pushing basement catfish and removes the primary rad onc from a key role of helping drive the patient's care plan. Or are rad oncs who have a primary disease site too dumb to assimilate new data on oligometastatic disease?
Can anyone tell me whether there are breast surgeons who only operate on right sided breast cancers but then refer to another breast surgeon if there is a suspicious node in the contralateral side? Or a med onc that only gives chemo when the the breast cancer is localized to the breast but when there is a spine met, a different med onc who is specially trained in metastatic disease gives the chemo?
Edit: Spacing of paragraphs.
Last edited: