- Joined
- Apr 3, 2019
- Messages
- 4,269
- Reaction score
- 9,961
This is an open-book, single question test.
Here is the book:
Here are the study guides:

Here is the book:
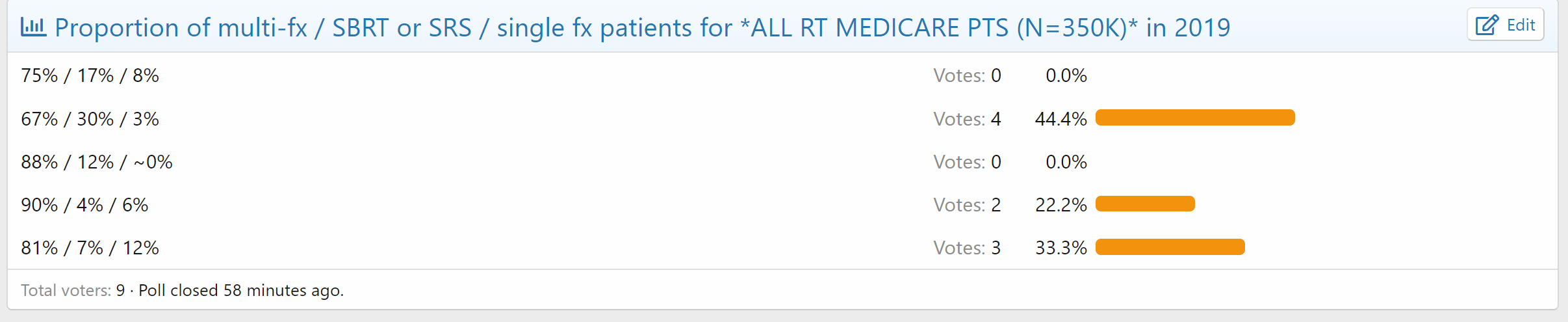
Centers for Medicare & Medicaid Services Data
data.cms.gov
Here are the study guides:

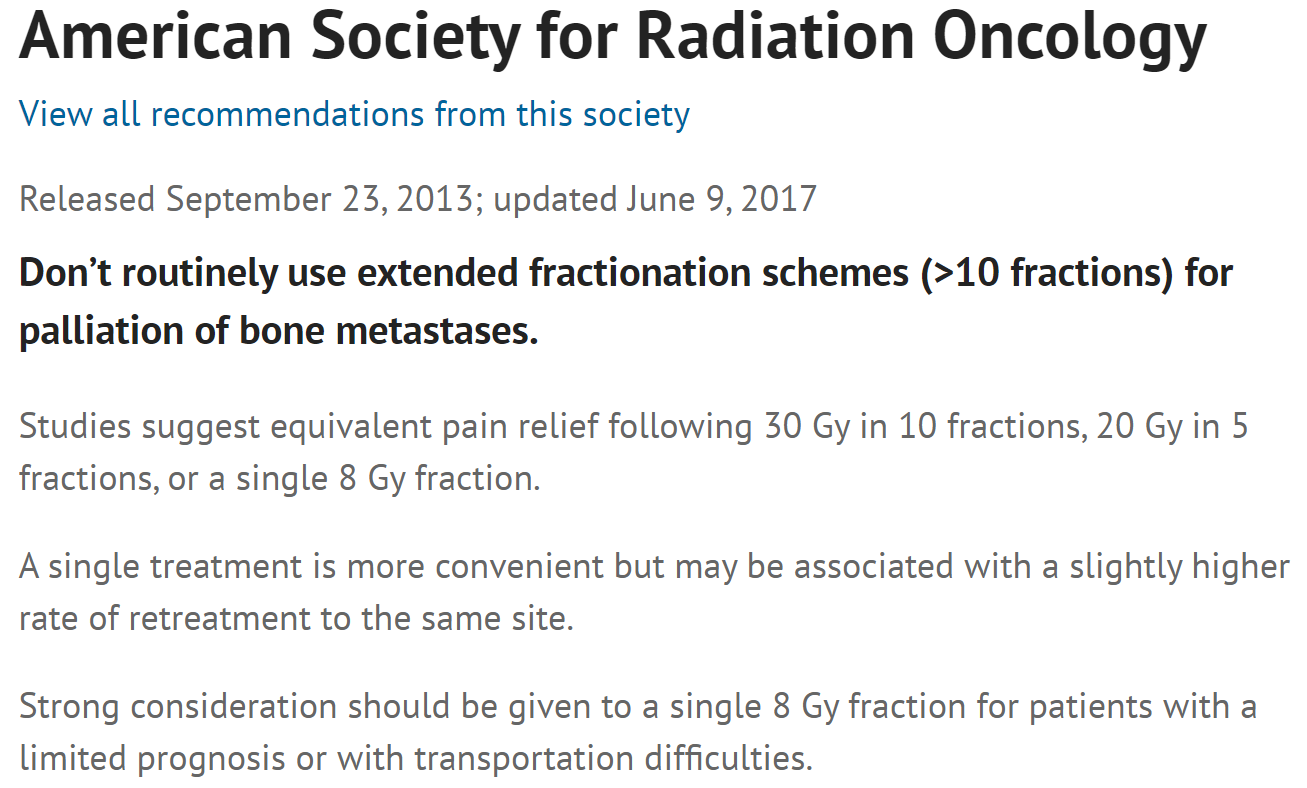
Single-Fraction RT for Bone Mets Should Be 'Standard'
In the first-ever 'real world' study of palliative radiotherapy for bone metastases, single and multiple fractions were equivalent.
www.medscape.com