TRALI incidence has decreased greatly since we moved from high volume crystalloid resuscitation to 1:1:1 product resuscitation.
Did you just quote best evidence from 23 years ago??? We have learned a lot about resuscitation since then thanks in no small part to at least 2 major wars fought in that time. Please review the trauma literature that’s come out since 1996. Massive blood loss is massive blood loss. Doesn’t matter if it was at the hands of a scalpel or bullet or MVA.
@SaltyDog, maybe i'm behind the times here... maybe there's a lot of new evidence i haven't heard of. Based on your remarks, am I to interpret the following?
1. That recent literature support transfusing well above 7 in a healthy surgical patient?
- American Association of Blood Banks (2016, JAMA) recommends restrictive RBC transfusion threshold of 7 g/dL for most hospitalized adult patients who are hemodynamically stable
- below 6-7 g/dL there is a significantly increase in cardiac output necessary to adequate perfuse end-organs
My practice - my GOAL Hgb is 7 for a healthy surgical patient, and my GOAL Hgb is higher for those with significant comorbidities. "GOAL" refers to end point. If a patient is bleeding briskly I TRANSFUSE earlier.
2. That recent literature support transfusing of FFP, cryoppt and platelets despite repeated, normal coagulation studies?
- then what's the point of sending and following coagulation labs if you're going to transfuse regardless of the result?
- The
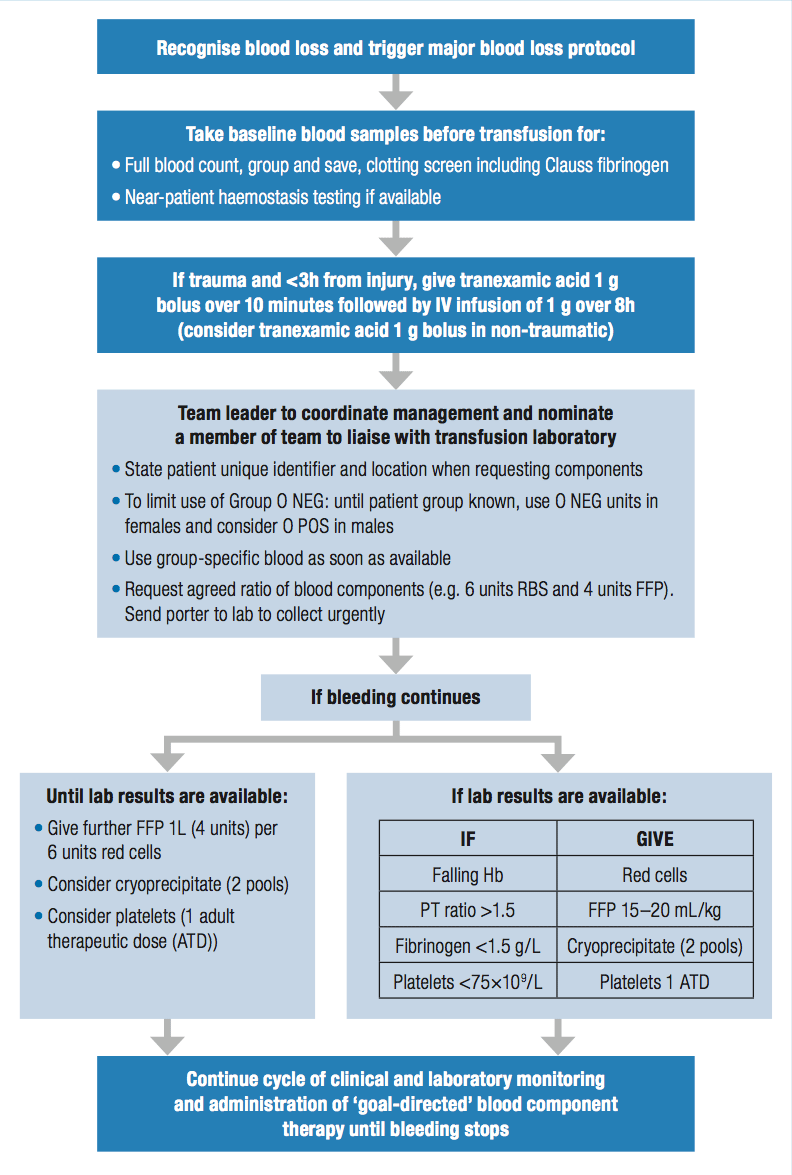
JPAC - Transfusion Guidelines as listed above for major hemorrhage is from 2013 onwards. It suggests initial resuscitation by transfusion ratios in an unstable patient, then transfusion directed based on lab results. Yes, it is from the UK. Maybe they have different management of hemorrhage. I can find some references from America, but as i remember it there aren't many differences.
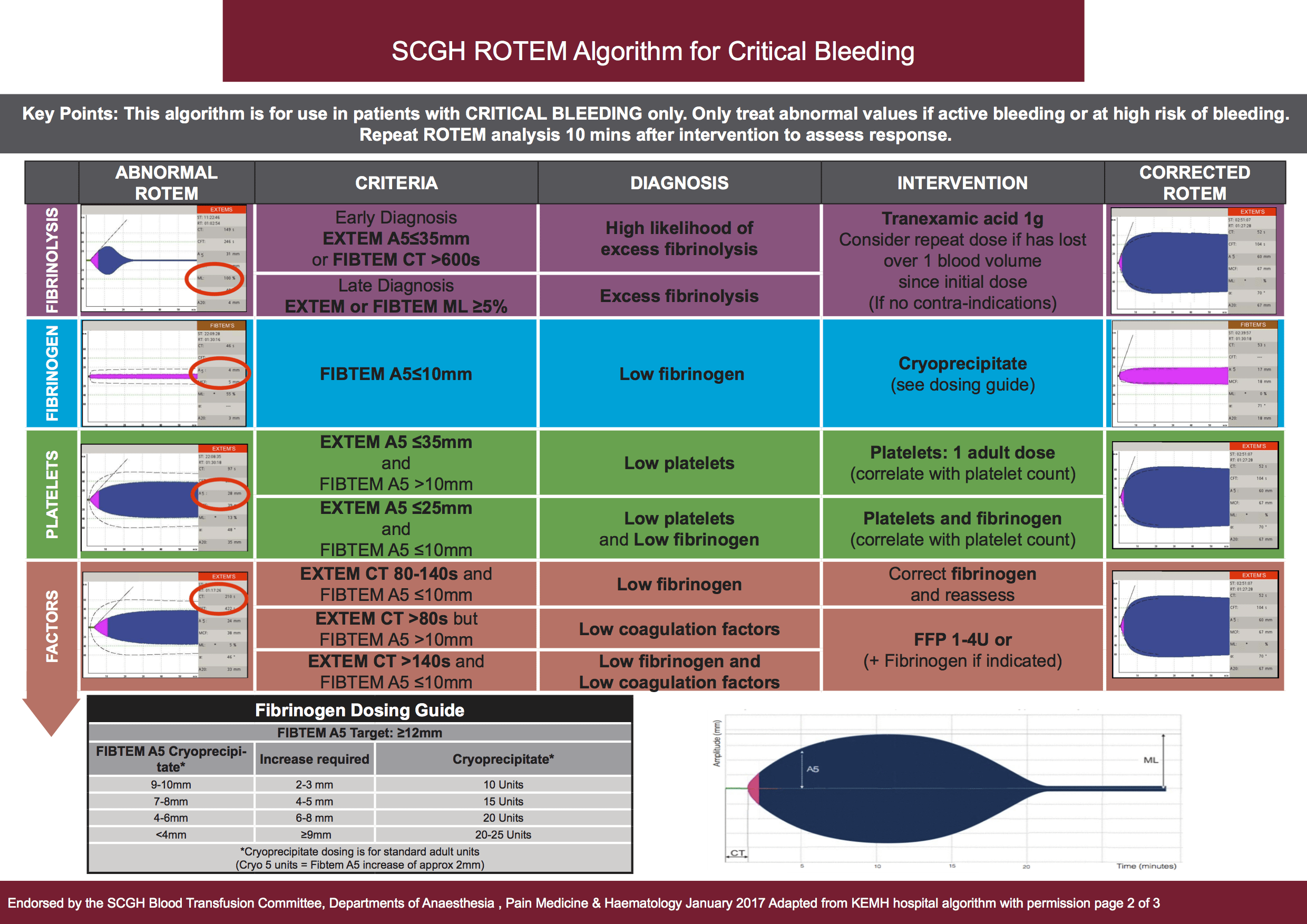
My practice - In the face of reliable, repeated, objective lab data showing no evidence of significant hypofibrinogemia, thrombocytopenia, or factor deficiency, I would offer TXA (Crash-2 Trial, Shakur et al., Lancet 2010) or DDAVP instead as the risk profile is lower
3. That there is any evidence that TRALI is caused by too much crystalloid and not due to transfusion of blood products?
- that giving 2 units of pRBC and fluids is MORE likely to cause TRALI than giving 2:2:2 pRBC:FFP: plt ? Seems unbelievable to me, since the "T" in TRALI stands for "transfusion", and the mechanisms involved (Fatalities Reported to FDA Following Blood Collection and Transfusion: Annual Summary for Fiscal Year 2015.
https://www.fda.gov/downloads/Biolo...m/TransfusionDonationFatalities/UCM518148.pdf)
My practice - I do not give empiric ratio therapy unless patient is hemorrhaging quickly and I need to volume resuscitate them. Otherwise I do lab-directed therapy. The risk of TRALI and other complications of transfusion increase with every unit of blood product administered.
How quickly blood loss occurs matters. Definitions of hemorrhage take into account the time course. A patient losing
3 liters in an hour does not respond the same as a patient losing
3 liters over 6 hours (and its not the same as a patient losing 3 liters over 6 days). The clinician's assessment and management should likewise be different. When I get a polytrauma, cold, hypovolemic, acidotic pt who has already bled out 3 liters, you bet I'm doing empiric transfusion ratios. The exact ratios are subject to continued study, e.g., 1:1:1 vs 1:1:2. etc... (PROPPR trial, 2015;
Transfusion in Patients With Severe Trauma), and yes in this particular situation there is evidence that using ratios is better-- although even this is debated.. (e.g., Fixed Ratio vs Goal Directed Therapy in Trauma Schochl et al., 2016; Effect of Fixed Ratio Transfusion protocol vs lab result guided transfusion in patients with severe trauma Nascimento et al., 2013; Change of transfusion and treatment paradigm in major trauma patients Stein et al., 2017) But when I have a carefully managed pt who has lost 3 liters over the course of many hours, hemodynamically stable, euvolemic, I'm doing lab-directed therapy not ratios. This should not be controversial.
Massive hemorrhage definitions often specify VOLUMES over TIMES: e.g., (i) blood loss exceeding circulating blood volume within a
24-hour period, (ii) blood loss of 50% of circulating blood volume within a
3-hour period, (iii) blood loss exceeding 150
ml/min, or (iv) blood loss that necessitates plasma and platelet transfusion [
3], although there is no universal definition. (Irita, KJA 2011)
Finally... I did
NOT "quote best evidence from 23 years ago". I referenced something from a textbook that is still considered a reasonable standard today, and which continues to be supported by expert opinion.
Again.. this seems incredibly intuitive to me, but am I missing something??