Appreciate the thoughtful discourse everyone. The thread got a little derailed at first and to be honest I contributed to that. Here is a quick summary on where I'm at on this matter, and briefly why it might be worth considering further. This is our bread and butter, probably highest % caseload of many practices. When you see a woman with a painful or disfigured breast, they are not happy. Any room for improvement should be considered, given the scale of treatment nationally and internationally.
Why 15 MIGHT be better than 16...
WHELAN: 612 women, 4256/16 vs 50/25, no boost, 10 year follow up
Local control: dead even
View attachment 323596
Cosmesis: dead even
View attachment 323597
Great study, practice changing, widely adopted with time.
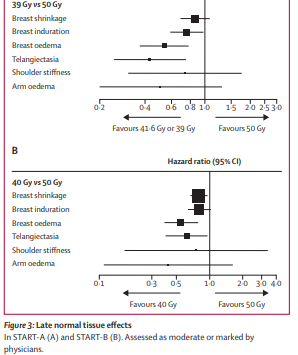
START B: 2215 women, STRAIGHT 1:1 randomization (no 2:2 or whatever everyone else is claiming, yes they lumped 2 studies in the 10 year pub but START B was its own thing) 50/25 vs 40/15, **boost allowed at treating MD discretion, even boost #s between arms, confounder.
Local control: Statistically dead even (crudely favored 40/15, not SS)
View attachment 323598
Cosmesis: SS favored hypofractionation significantly
View attachment 323599
Many more patients that Whelan, at least equal tumor control, impressive improvement in cosmesis, boost allowed. New standard? Improvement on Whelan?
FAST FORWARD: 4096 women, 1:1:1 rando to 40/15, 27/5, or 26/5. 5 year follow up.
Local control: dead even
View attachment 323600
Cosmesis: Clearly worse for 27/5, somewhat comparable for 26/5 vs 40/15, but some factors superior for 40/15
View attachment 323601
As
@scarbrtj has said, the therapeutic window for radiotherapy can be annoyingly small. Seriously, 1Gy makes the difference?? Also, to
@evilbooyaa credit, the brits were way too willing to gloss over some of the differences between 40/15 and 26/5 in issues such as breast induration, telangiectasia, and breast/chest wall (o)edema to further their agenda of decreased utilization.
SUMMARY
Whelan: was a practice changing study and remains a go to standard in US and Canada. Same outcome, less treatments.
START B: essentially one less fraction than Whelan, replicated Whelan otherwise and proved no detriment in tumor control with improved cosmesis. Allowed boost which is a bit of a confounder. We know boost is detrimental to cosmesis.
FAST FORWARD: 40/15 still looked like the winner to me. And shocking difference between 27/5 and 26/5. If one gray can make all the difference is this large phase 3 study, couldn't an additional 2.6 Gy fraction of whole breast radiation be the difference maker in cosmesis between 40/15 and 42.56/16?
FINAL TAKEAWAYS:
- I have no life and like to ponder pathetic questions like whole breast in 15 vs 16
- There might be a small toxicity difference between the two and given the scale of the diagnosis and treatment, its worth considering further even if it seems too basic
- If you are looking for the cleanest data without a boost, its Whelan
- If you want to boost, consider 40/15 as the whole breast portion