- Joined
- Jan 26, 2017
- Messages
- 87
- Reaction score
- 218
Cant post something like this on twitter because /cancelled so posting here but does an ounce of prevention really equal a pound of cure? Docs and lay public alike often treat screening as prima facie
Discuss.
 jamanetwork.com
jamanetwork.com
JAMA Intern Med. 2023 Aug 28.
doi: 10.1001/jamainternmed.2023.3798. Online ahead of print.
Estimated Lifetime Gained With Cancer Screening Tests: A Meta-Analysis of Randomized Clinical Trials
Michael Bretthauer 1, Paulina Wieszczy 1 2, Magnus Løberg 1, Michal F Kaminski 1 2 3, Tarjei Fiskergård Werner 4, Lise M Helsingen 1, Yuichi Mori 1 5, Øyvind Holme 1, Hans-Olov Adami 1 6 7, Mette Kalager 1
PMID: 37639247 DOI: 10.1001/jamainternmed.2023.3798
Abstract
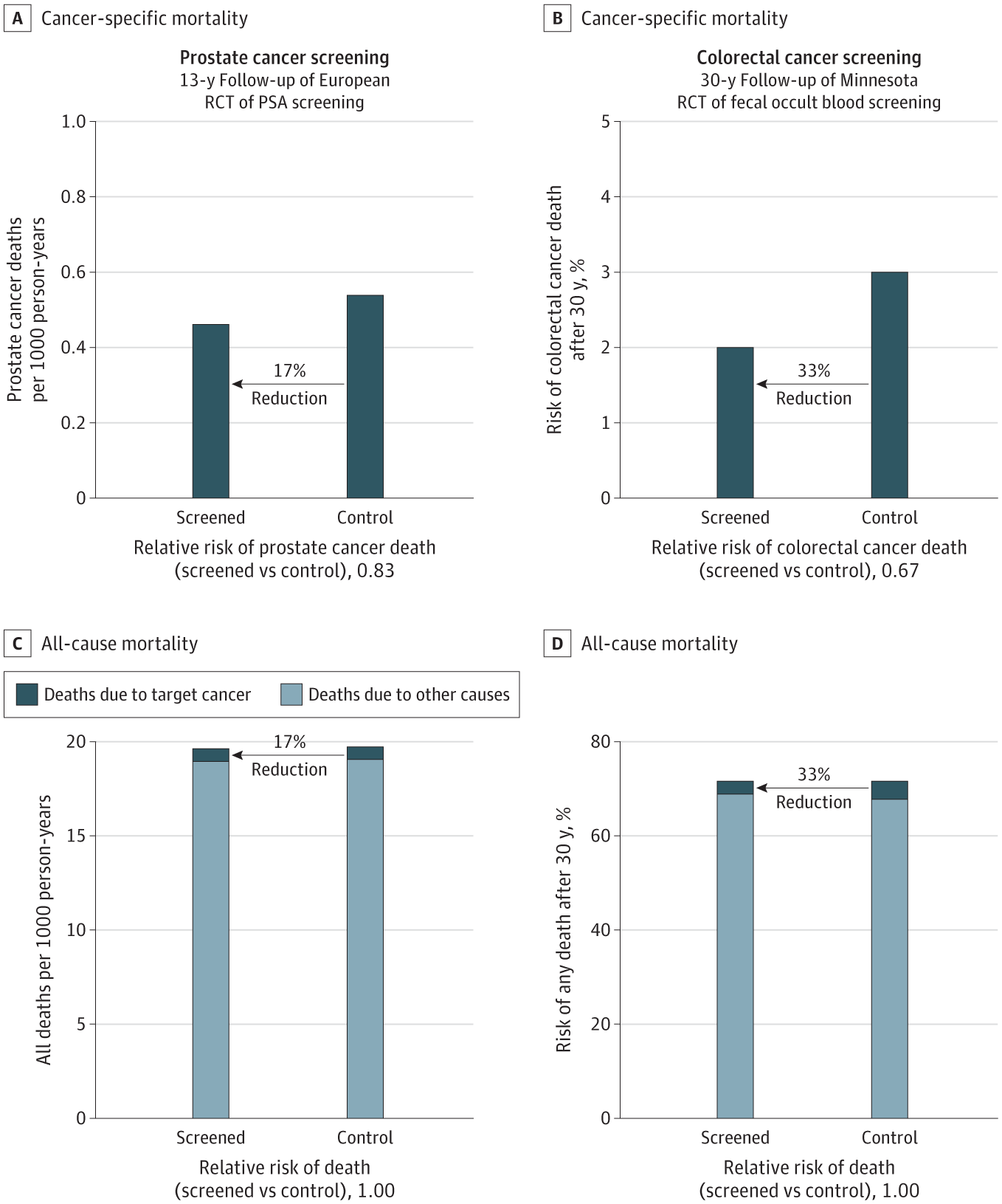
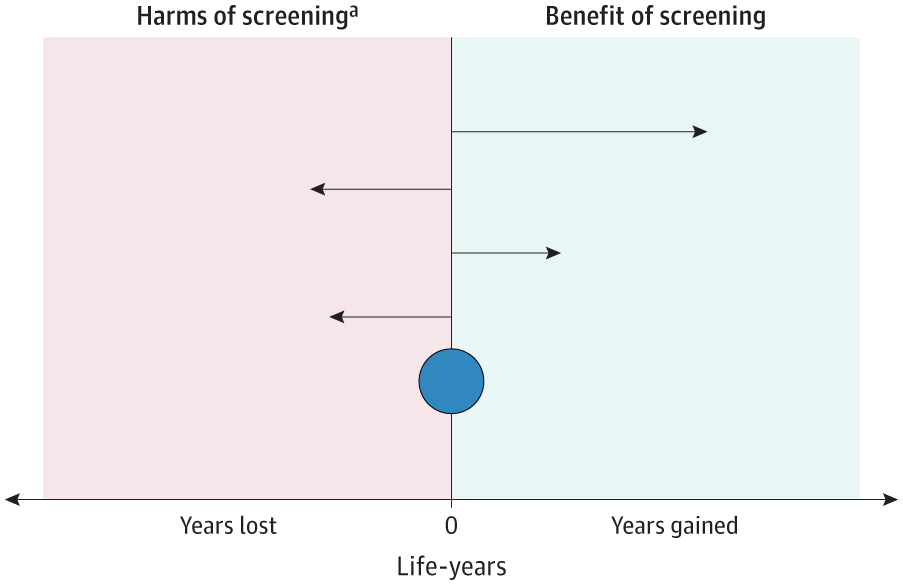
Importance: Cancer screening tests are promoted to save life by increasing longevity, but it is unknown whether people will live longer with commonly used cancer screening tests.
Objective: To estimate lifetime gained with cancer screening.
Data sources: A systematic review and meta-analysis was conducted of randomized clinical trials with more than 9 years of follow-up reporting all-cause mortality and estimated lifetime gained for 6 commonly used cancer screening tests, comparing screening with no screening. The analysis included the general population. MEDLINE and the Cochrane library databases were searched, and the last search was performed October 12, 2022.
Study selection: Mammography screening for breast cancer; colonoscopy, sigmoidoscopy, or fecal occult blood testing (FOBT) for colorectal cancer; computed tomography screening for lung cancer in smokers and former smokers; or prostate-specific antigen testing for prostate cancer.
Data extraction and synthesis: Searches and selection criteria followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline. Data were independently extracted by a single observer, and pooled analysis of clinical trials was used for analyses.
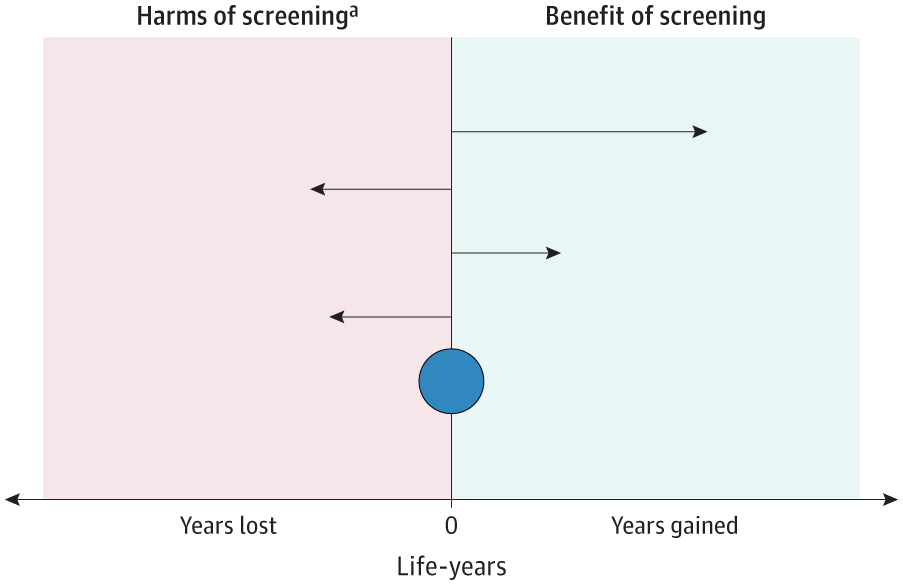
Main outcomes and measures: Life-years gained by screening was calculated as the difference in observed lifetime in the screening vs the no screening groups and computed absolute lifetime gained in days with 95% CIs for each screening test from meta-analyses or single randomized clinical trials.
Results: In total, 2 111 958 individuals enrolled in randomized clinical trials comparing screening with no screening using 6 different tests were eligible. Median follow-up was 10 years for computed tomography, prostate-specific antigen testing, and colonoscopy; 13 years for mammography; and 15 years for sigmoidoscopy and FOBT. The only screening test with a significant lifetime gain was sigmoidoscopy (110 days; 95% CI, 0-274 days). There was no significant difference following mammography (0 days: 95% CI, -190 to 237 days), prostate cancer screening (37 days; 95% CI, -37 to 73 days), colonoscopy (37 days; 95% CI, -146 to 146 days), FOBT screening every year or every other year (0 days; 95% CI, -70.7 to 70.7 days), and lung cancer screening (107 days; 95% CI, -286 days to 430 days).
Conclusions and relevance: The findings of this meta-analysis suggest that current evidence does not substantiate the claim that common cancer screening tests save lives by extending lifetime, except possibly for colorectal cancer screening with sigmoidoscopy.
Discuss.
Estimated Lifetime Gained With Cancer Screening Tests
The meta-analysis examines evidence from randomized clinical trials of lifetime gained with use of screening tests for lung, breast, prostate, and colorectal cancer.
JAMA Intern Med. 2023 Aug 28.
doi: 10.1001/jamainternmed.2023.3798. Online ahead of print.
Estimated Lifetime Gained With Cancer Screening Tests: A Meta-Analysis of Randomized Clinical Trials
Michael Bretthauer 1, Paulina Wieszczy 1 2, Magnus Løberg 1, Michal F Kaminski 1 2 3, Tarjei Fiskergård Werner 4, Lise M Helsingen 1, Yuichi Mori 1 5, Øyvind Holme 1, Hans-Olov Adami 1 6 7, Mette Kalager 1
PMID: 37639247 DOI: 10.1001/jamainternmed.2023.3798
Abstract
Importance: Cancer screening tests are promoted to save life by increasing longevity, but it is unknown whether people will live longer with commonly used cancer screening tests.
Objective: To estimate lifetime gained with cancer screening.
Data sources: A systematic review and meta-analysis was conducted of randomized clinical trials with more than 9 years of follow-up reporting all-cause mortality and estimated lifetime gained for 6 commonly used cancer screening tests, comparing screening with no screening. The analysis included the general population. MEDLINE and the Cochrane library databases were searched, and the last search was performed October 12, 2022.
Study selection: Mammography screening for breast cancer; colonoscopy, sigmoidoscopy, or fecal occult blood testing (FOBT) for colorectal cancer; computed tomography screening for lung cancer in smokers and former smokers; or prostate-specific antigen testing for prostate cancer.
Data extraction and synthesis: Searches and selection criteria followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline. Data were independently extracted by a single observer, and pooled analysis of clinical trials was used for analyses.
Main outcomes and measures: Life-years gained by screening was calculated as the difference in observed lifetime in the screening vs the no screening groups and computed absolute lifetime gained in days with 95% CIs for each screening test from meta-analyses or single randomized clinical trials.
Results: In total, 2 111 958 individuals enrolled in randomized clinical trials comparing screening with no screening using 6 different tests were eligible. Median follow-up was 10 years for computed tomography, prostate-specific antigen testing, and colonoscopy; 13 years for mammography; and 15 years for sigmoidoscopy and FOBT. The only screening test with a significant lifetime gain was sigmoidoscopy (110 days; 95% CI, 0-274 days). There was no significant difference following mammography (0 days: 95% CI, -190 to 237 days), prostate cancer screening (37 days; 95% CI, -37 to 73 days), colonoscopy (37 days; 95% CI, -146 to 146 days), FOBT screening every year or every other year (0 days; 95% CI, -70.7 to 70.7 days), and lung cancer screening (107 days; 95% CI, -286 days to 430 days).
Conclusions and relevance: The findings of this meta-analysis suggest that current evidence does not substantiate the claim that common cancer screening tests save lives by extending lifetime, except possibly for colorectal cancer screening with sigmoidoscopy.