Long post alert! I've found myself doing several awake cranis out in PP (not my fave, but the surgeon often requests me... yuck). Most important is having a cooperative and motivated patient, and of course the heavier they are (+ OSA) makes it more challenging. I've found surgeons know this and do a reasonable job at screening beforehand who is a good candidate.
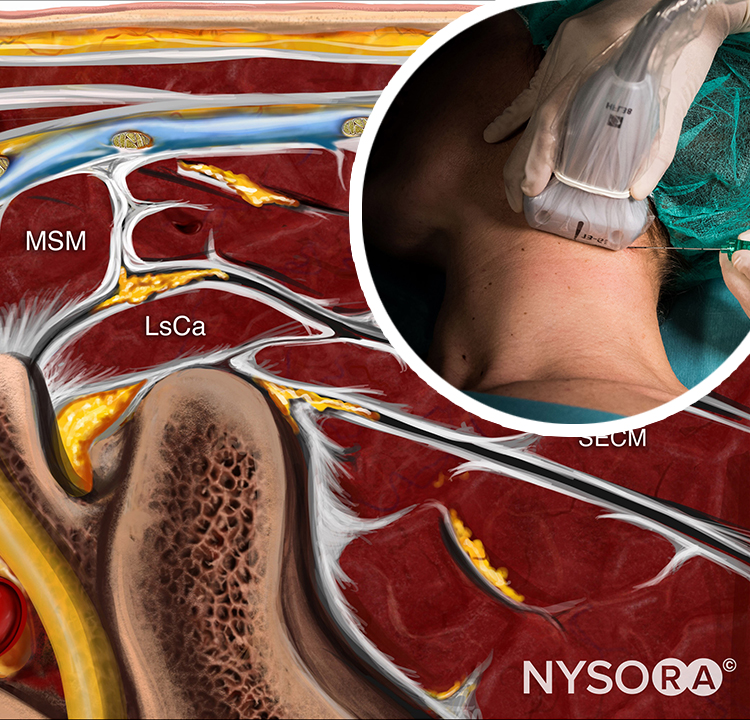
Doing it as an "all awake" approach (MAC-Awake) technique is common but I never had much success with it, personally. My preferred technique I learned in training is "Asleep-Awake-Asleep" or just MAC after the awake portion if preferred. No premedication other than 0.1-0.2 mg Glyco as an antisialogogue (you want them to wake up somewhat quickly) and start with scalp blocks - I do them myself in my practice but you'll need to find a "control" syringe so you can aspirate. You can't inject too much volume under skin so I do a 10 mL mixture of 1/2 Mepivacaine (2 or 3%) and 1/2 ropivacaine (0.5%). Here's the technique and landmarks in this paper:
https://pdfs.semanticscholar.org/3be4/3a2edb665bba2024e99de375f4fb6d6cb238.pdf
After that I'll induce (propofol only) and place an LMA and pre-hook up a NC with ETCO2 capability and run 0.5 MAC Sevo (nearly the only time I run it for a neuro case) and run 0.1 mcg/kg/min Remi (more if a chronic narcotic user). An alternative is substituting Precedex (0.5-0.75 mcg/kg/hr with no bolus, but start it early) +/- propofol for inhalation agent and keep it TIVA, this also works well. The stimulating portions are head pinning and craniotomy - with good scalp blocks there shouldn't be a tremendous amount of hemodynamic change. Once the dura is opened the surgeon usually lets me know he'll want the patient awake soon - I'll cut off the gas and turn back the Remi to 0.05. Or you can turn off the propofol and turn back the Precedex to 0.25-0.5, this also works well. I have found that patients do require a very mild plane of sedation to stay calm during surgery. My partners like to turn it all off and there have been some incidents in the past. Usually these patients emerge with a "Remi" wakeup - awaken to voice and I slip out the LMA and turn on 2-4L O2 via NC. I'll keep the patient the calm, explain what is happening, and call over the neuropsych team.
I'll see how the patient handles the awake portion and if it goes super smoothly and is tolerated well I'll just double the infusions after the resection is complete (Precedex is great here). If the patient requests or I am uncomfortable I'll bolus propofol and slip the LMA back in.
Pitfalls: Giving significant amounts of versed and fentanyl will delay your wakeup and provide a very poorly-cooperative patient during that process. Avoid them and lean more on Remi if you need narcotic.
- Incomplete anesthesia of the scalp - discuss craniotomy and pin locations with surgeon ahead of time.
- Obesity/OSA - these are the most difficult awake cases, lean more on Precedex here and less on narcotic.
For those of us in ACT practices and have an anesthetist in the room - you need someone comfortable and facile with this sort of plan and able to adjust sedation quickly and that you can trust to keep you in the loop. I spend a LOT of time in these rooms, probably among my most hands-on. Go over the plan ahead of time, hopefully the day before if you can. These cases are not where you want brand new hires, a CA-1 still working out the basics of anesthesia, or a locums anesthetist who's been doing simple general surgery for 10+ years. I always choose my anesthetist ahead of time personally and the cases have gone well for me so far in my short career.
Hope this has been helpful to folks out there! Just like any other surgery there are many ways to do the anesthesia for this case, what I described works great for my personal practice and experience but I am constantly tweaking things (reading up more on scalp anatomy, incorporating Precedex as it becomes much more readily available).