- Joined
- Dec 17, 2007
- Messages
- 3,383
- Reaction score
- 4,390
Here is a challenging NSCLC case.
75 year old patient, good PS.
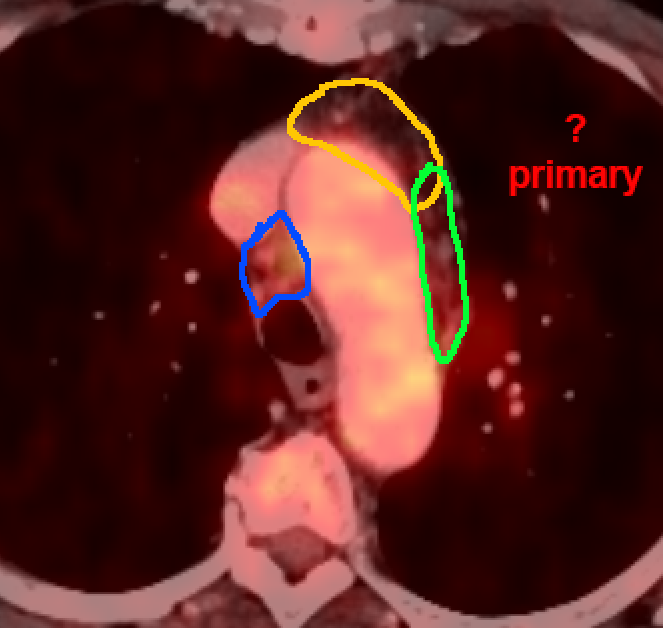
Small primary in the left lung, mediastinum looks mostly clear on PET, only a few very small nodes. MRI of the brain shows solitary <1cm lesion.
Histology come backs as adenocarcinoma in the lung, EGFR-mutated.
I just SRSed the brain lesion (EGFR-mutation was not known prior to the planning CT ).
).
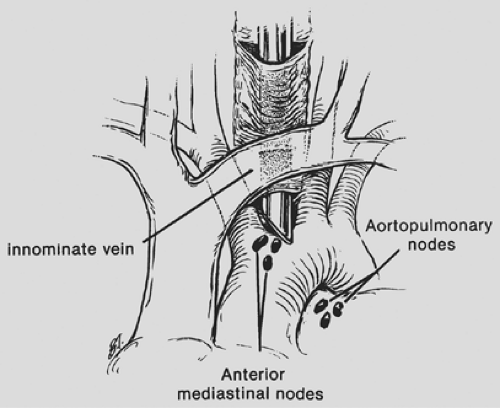
The thoracic surgeons performed a mediastinoscopy this week to rule out any mediastinal involvement, they resected two nodes, which came back positive in the right mediastinum (with only minor involvement). So, it's a cT1c cN3 cM1 (BRA; solitary).
What to do?
Possible alternatives:
1. It's cN3 cM1. Give the patient Tagrisso and call it a day until progression occurs (hopefully in several years).
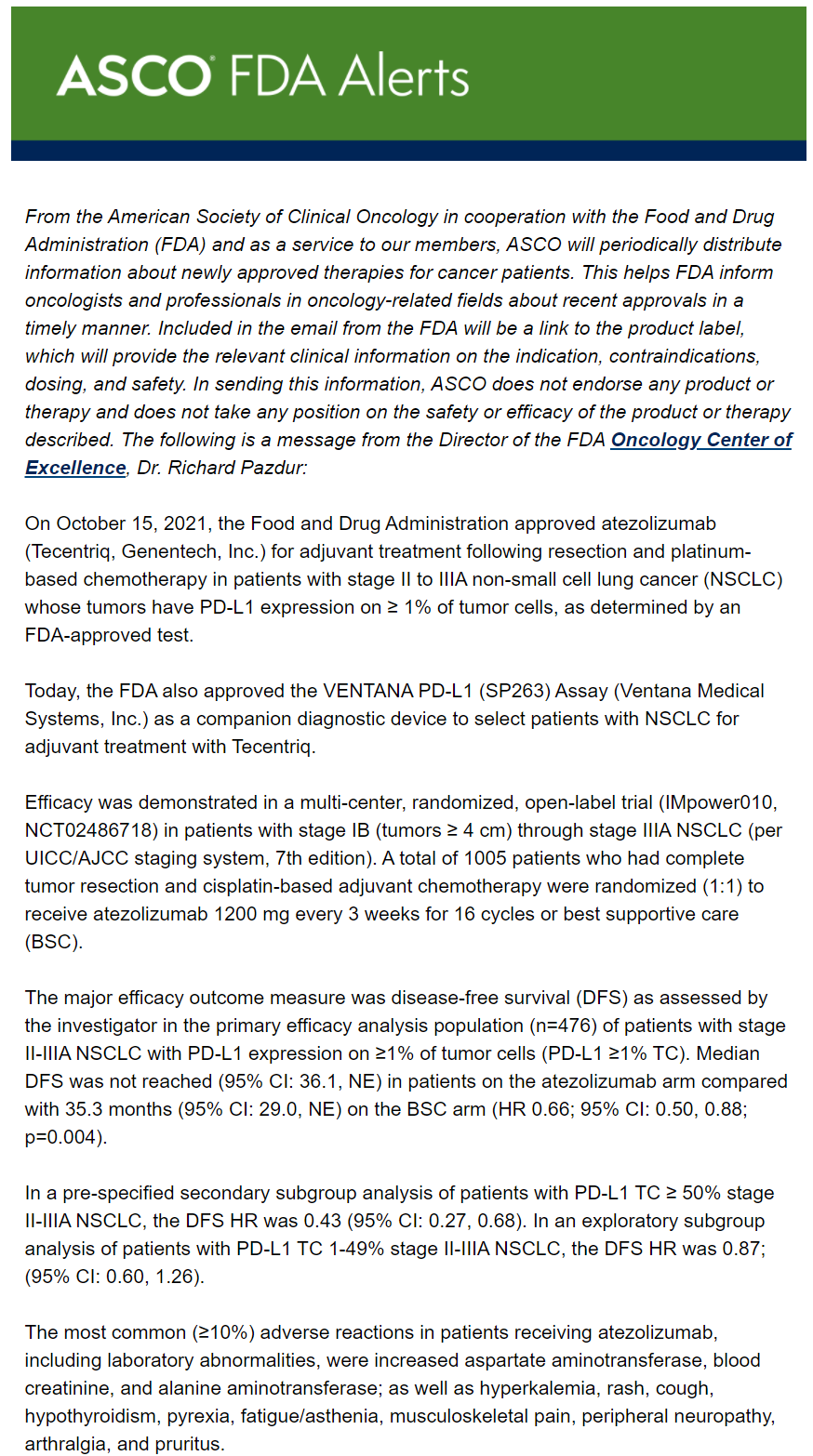
2. We just killed the met, so let's go for The Full Monty! Concurrent radiochemotherapy for the primary and mediastinum, add Tagrisso as adjuvant treatment (extrapolated from ADAURA).
3. Re-PET, if the mediastinum looks clear after the mediastinoscopy, then SBRT the primary and give Osimertinib.
75 year old patient, good PS.
Small primary in the left lung, mediastinum looks mostly clear on PET, only a few very small nodes. MRI of the brain shows solitary <1cm lesion.
Histology come backs as adenocarcinoma in the lung, EGFR-mutated.
I just SRSed the brain lesion (EGFR-mutation was not known prior to the planning CT
The thoracic surgeons performed a mediastinoscopy this week to rule out any mediastinal involvement, they resected two nodes, which came back positive in the right mediastinum (with only minor involvement). So, it's a cT1c cN3 cM1 (BRA; solitary).
What to do?
Possible alternatives:
1. It's cN3 cM1. Give the patient Tagrisso and call it a day until progression occurs (hopefully in several years).
2. We just killed the met, so let's go for The Full Monty! Concurrent radiochemotherapy for the primary and mediastinum, add Tagrisso as adjuvant treatment (extrapolated from ADAURA).
3. Re-PET, if the mediastinum looks clear after the mediastinoscopy, then SBRT the primary and give Osimertinib.