Hi Simul,
Again, I appreciate the thoughtful comments that you and everyone have been bringing. I’m glad that we can have a conversation where we don’t all agree with each other, but still can have an exchange of ideas to help understand each other’s perspective to ultimately help improve our field. Like I said from the beginning, I’m not here to try to change opinions about rad onc or about my program. But I am here to listen and try to work to improve our residency and the training experience for our residents at Columbia.
As you and the SDN community are focused on always be contracting as one approach to help our field, I am focused on creating new training pathways to foster individualized talent and create new types of leaders. This includes developing and celebrating people who “just” want to be great doctors, which is frankly the most important thing we do.
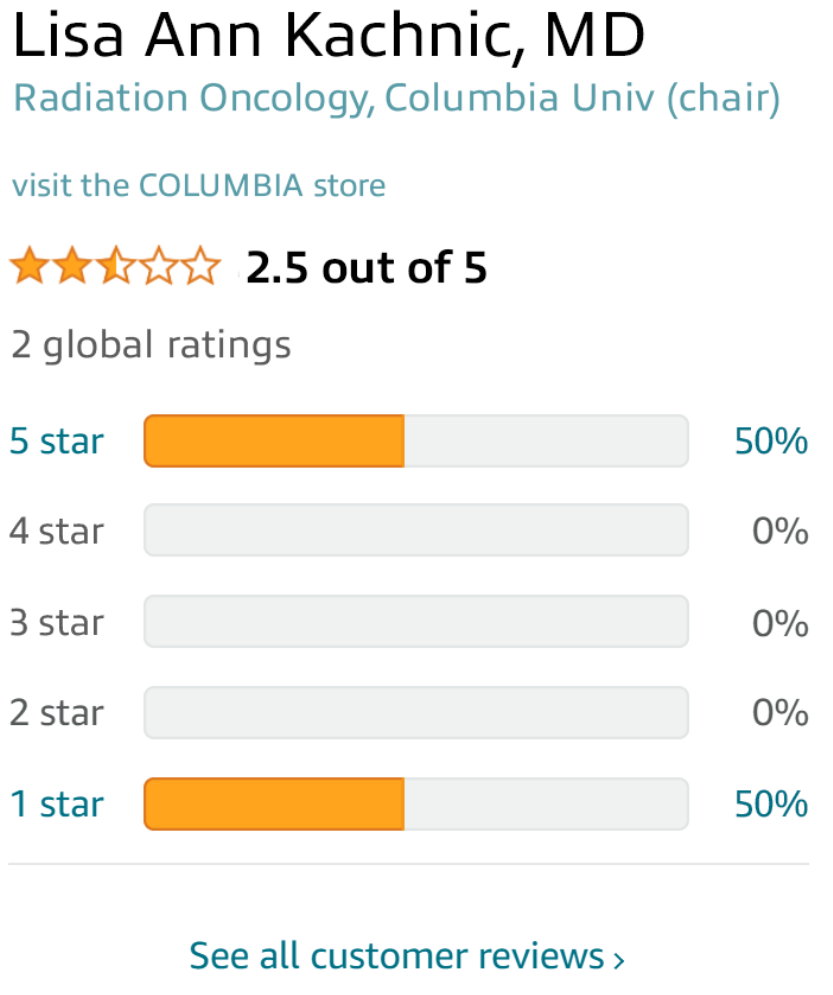
I agree with you that creating new training pathways, developing the next generation of leaders, and expansion do NOT have to go hand in hand. I have actually been working with Dr. Kachnic and the residents at Columbia, and we will contract our residency from 8 to 7 until the current environment improves. Having taken this step, what we do need is help from you and other private practice rad oncs, in addition to chairs and other PDs, to work with us to develop a curriculum or pathway for those who want to go into the community to be the best damn doctors possible. Trainees wanting to be extraordinary in patient care should have a “Namloh” pathway to celebrate and develop their passion, as research scientists have with Holman.
I like your recommendation of going back to the basics and I have already implemented changes that I have control over. The APD and I have reached out to some colleagues in the community and have received helpful recommendations, including developing a practical Physics/Dosi/QA curriculum, a billing/coding and APM literacy program, a practical leadership development series, and building a support network of alumni in the community to help residents. But we need more.
I agree the conversation on the blog is changing so let’s talk offline. I need your help and the help of anyone else who wants to try to be part of the solution. Having the narrow view of someone who has stayed in academia, I know I will need help from the community for broad perspectives if the goal is to improve training for real success in all aspects of post-residency practice. I hope to hear from you in the near future. Feel free to email me at your earliest convenience. And anyone else who wants to join as we work constructively, please email me at
[email protected].
Thanks,
David