Hi SDN friends,
I would like to run by you all a difficult Lymphoma case.
40 year old male when presented with Fevers, is diagnosed with DLBCL with bulky 11.3 cm para-aortic mass, cervical, axillary, Supra-clavicular, mediastianal, bilateral common iliac, bilateral internal and external iliac Lymphoma masses. Largest mediastinal (Sub-carinal and left para-tracheal) is 2 x 0.8 cm with SUV uptake of 9.3.
After 3 cycles of R-CHOP, interim PET/CT showed excellent response with resolution of all FDG avid masses except mediastinum with activity in paratracheal, and sub-carinal nodes with largest node measuring 1.7 x 1.0 cm with SUV of 5.0. After 6 cycles of R-CHOP, Right para-tracheal node is 8 mm with SUV of 6.36 and Sub-cardinal node of 10 mm with SUV of 5.26.
Hematologist thinks these residual uptake in these mediastinal lymph nodes is not significant or maybe due to inter-current infections. Since the size of these mediastinal lymph nodes is smaller, Heam/Onc thinks no residual disease in these lymph nodes. Pt says he had some symptoms of URI, cough before both PET/CT. So Hematologist doesn’t want to consider him for high dose Chemotherapy with autologous BMT and referred him for radiation to originally bulky region that is para-aortic nodal region only. Heam/Onc wants to consider him for BMT if follow up PET/CT or CT shows increase in the size of these mediastinal nodes. So Pt is also not interested in BMT now.
Heam/Onc asked not to include mediastianal nodes in the radiation field.
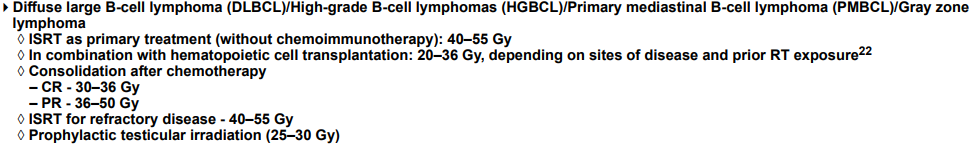
I personally think the residual uptake in these mediastinal nodes is significant and want to do mediastinal RT to 45Gy and Para-Aortic RT to 36Gy.
Questions.
1. Is it reasonable omit radiation to mediastinal lymph nodes?
2. What is the benefit of radiation to these PA (completely FDG resolution) originally bulky nodes if pt ends up needing BMT eventually?
Thanks a lot!
I would like to run by you all a difficult Lymphoma case.
40 year old male when presented with Fevers, is diagnosed with DLBCL with bulky 11.3 cm para-aortic mass, cervical, axillary, Supra-clavicular, mediastianal, bilateral common iliac, bilateral internal and external iliac Lymphoma masses. Largest mediastinal (Sub-carinal and left para-tracheal) is 2 x 0.8 cm with SUV uptake of 9.3.
After 3 cycles of R-CHOP, interim PET/CT showed excellent response with resolution of all FDG avid masses except mediastinum with activity in paratracheal, and sub-carinal nodes with largest node measuring 1.7 x 1.0 cm with SUV of 5.0. After 6 cycles of R-CHOP, Right para-tracheal node is 8 mm with SUV of 6.36 and Sub-cardinal node of 10 mm with SUV of 5.26.
Hematologist thinks these residual uptake in these mediastinal lymph nodes is not significant or maybe due to inter-current infections. Since the size of these mediastinal lymph nodes is smaller, Heam/Onc thinks no residual disease in these lymph nodes. Pt says he had some symptoms of URI, cough before both PET/CT. So Hematologist doesn’t want to consider him for high dose Chemotherapy with autologous BMT and referred him for radiation to originally bulky region that is para-aortic nodal region only. Heam/Onc wants to consider him for BMT if follow up PET/CT or CT shows increase in the size of these mediastinal nodes. So Pt is also not interested in BMT now.
Heam/Onc asked not to include mediastianal nodes in the radiation field.
I personally think the residual uptake in these mediastinal nodes is significant and want to do mediastinal RT to 45Gy and Para-Aortic RT to 36Gy.
Questions.
1. Is it reasonable omit radiation to mediastinal lymph nodes?
2. What is the benefit of radiation to these PA (completely FDG resolution) originally bulky nodes if pt ends up needing BMT eventually?
Thanks a lot!