- Joined
- Nov 21, 1998
- Messages
- 13,308
- Reaction score
- 7,973
- Points
- 8,231
- Location
- Over the rainbow
- Attending Physician
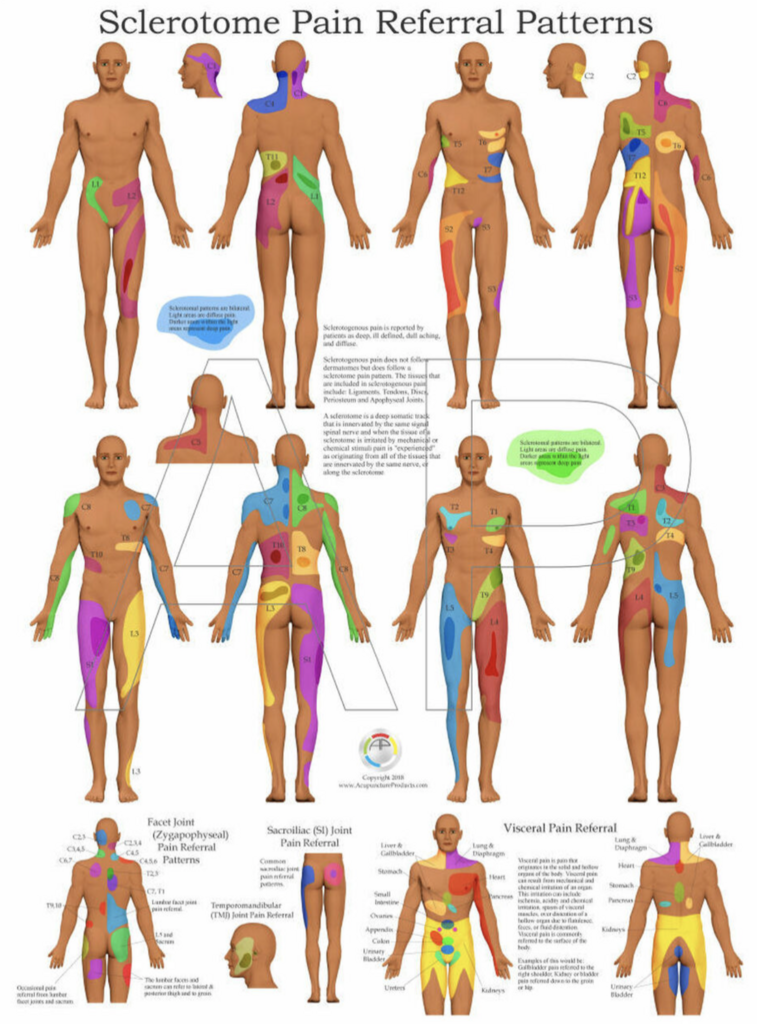
Any endplate changes? This sounds like a textbook case of "vertebrogenic" back pain with sclerotomal referral. I've heard that Intracept has been good.
 www.spineuniverse.com
www.spineuniverse.com
Chronic Low Back Vertebrogenic Pain Involves the Spinal Vertebral Endplates
Chronic low back pain research shows the lumbar vertebral endplates can cause vertebrogenic pain and involve the basivertebral nerve (BVN). How BVN pain is diagnosed and treated using BVN nerve ablation.
