- Joined
- Jul 12, 2004
- Messages
- 5,278
- Reaction score
- 4,969
90 yo F comes to ED with AMS.
Do you think there is electrocardiographic evidence of STEMI?
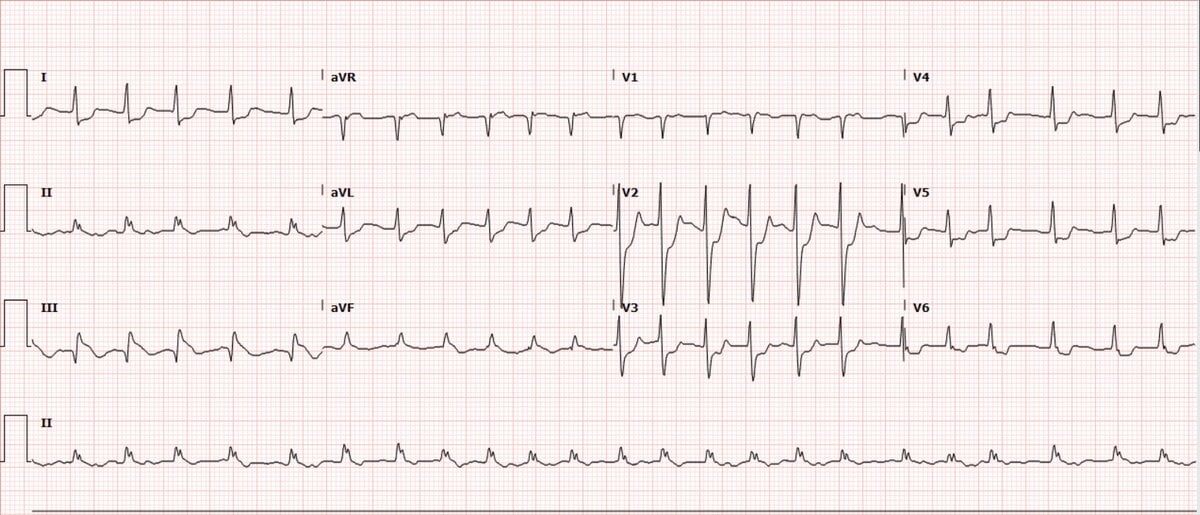
Do you think there is electrocardiographic evidence of STEMI?
HR initially 136, RR 22, BP 131/90, SpO2 96% RA. Temp 103. FSG normal
Cursory exam: Pt is very altered but mumbling words. She doesn't know if she is having chest pain. She looks terrible. No other med history available right now.
Cursory exam: Pt is very altered but mumbling words. She doesn't know if she is having chest pain. She looks terrible. No other med history available right now.
Cr 2, K+ 6.9, Bicarb 21, Trop 0.035 ng/ml, Lactic 3.3, WBC 15, Hg 14
Cardiologist says not a STEMI, doesn't see elevation in the inferior leads except III
For what it's worth, I thought it was a STEMI. While I don't necessarily think she would go to cath given her high fever, age, to me it's a STEMI on cath. I annotated the EKG as such:
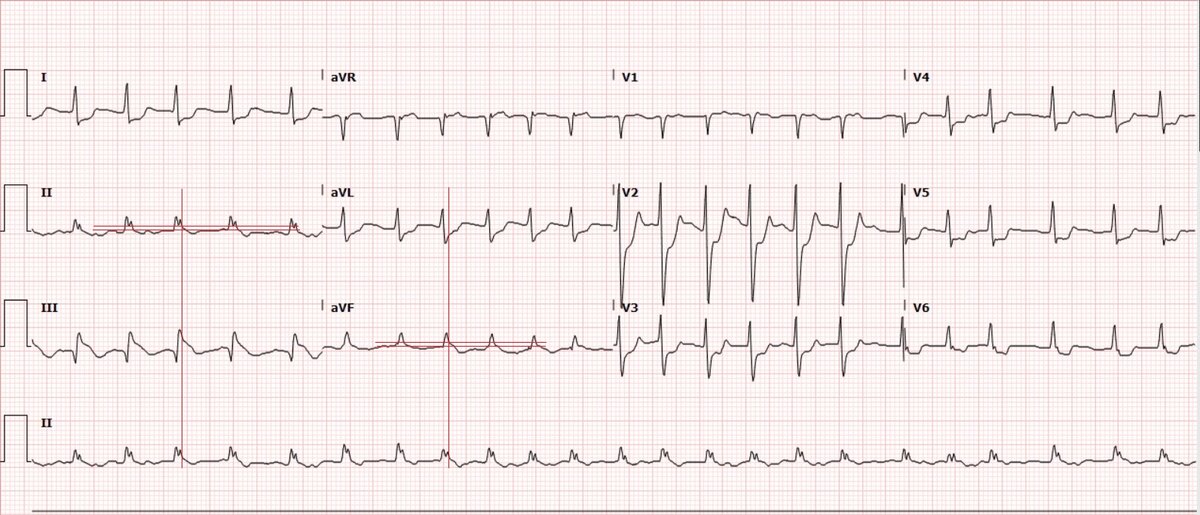
And when you zoom in on II, aVF....
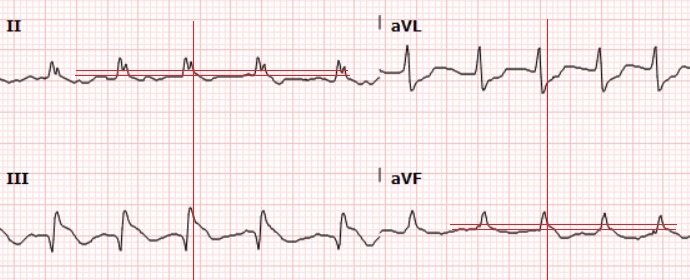
Those look like inferior elevations to me.
So far...nothing bad has happened to her on the floor. Looks like they are not even cycling her troponins. No cardiology consult noted. So maybe I am wrong...wanted your opinion.
And when you zoom in on II, aVF....
Those look like inferior elevations to me.
So far...nothing bad has happened to her on the floor. Looks like they are not even cycling her troponins. No cardiology consult noted. So maybe I am wrong...wanted your opinion.
