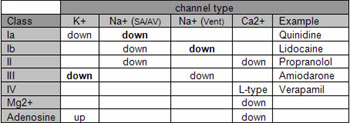
Awesome question with a cool answer. Unfortunately, it requires some detail to explain. Here's a table I made when I was
sorting it out for myself.
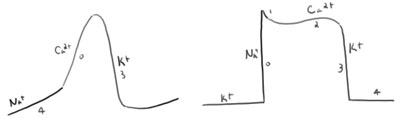
The Na+ channels of the SA and AV nodes are always firing (more or less) and are termed "active". This is in contrast to the Na+ channels of the ventricles that are usually off or "inactive". This all makes sense when you remember that the slow depolarization of the SA/AV is via Na+ channel, whereas the Na+ channels of the ventricles are off except for a very brief phase 0 upstroke (not a lot of time for a drug to take effect).
So, what makes a Class I a Class I is its action on these active Na+ channels. From this, you expect their action to be in the nodes and not in the ventricles. What makes Quinidine a Ia is its additional K+ action. In the SA/AV, this would prolong repolarization. In the ventricles, this would also prolong repolarization. Now, the prolonged QT, the slowing HR, etc begin to make sense.
If you can keep the differences between the SA/AV and the Ventricles straight AND commit the table I included to memory, then the effects of these drugs start to come together. Shockingly, more detail up front requires less memorization later on and leads to a real understanding of antiarrhythmials.
So when people say that Amiodarone is also a Class I, they're missing it! Amiodarone doesn't have the basic action that makes a Class I a Class I, and instead includes the actions that make a Ia and a Ib different from a standard Class I.
Lot of details, but interesting nonetheless. The only thing I'll add is that the Na+ channel in the SA/AV is a "funny" channel and that the Ca2+ channel in the SA/AV is an L-type channel. Why do you care? Well, the actions of Beta-Blockers don't make sense otherwise. Beta-blockers like Propranolol can act at the Funny channel and the L-type channels in the SA/AV, and can also act at the Ca2+ in the ventricle, but you don't see them affect the Na+ channel in the ventricles.
You should be able to piece together the rest. In the meantime, here are the bullet points.
Block: Effect
K+: Delays repolarization ↑AP duration, ↑ ERP, ↑ QT interval (risk for Torsade de pointes)
Na+ (SA/AV): ↓ automaticity, ↓ slope of phase 4, ↓ cell excitability
Na+ (Vent) : ↓ conduction, ↓ slope of phase 0 depolarization
Ca2+: ↓ conduction (SA/AV), ↓ slope of phase 4, ↓ phase 2 plateau (Vent), ↓ contractility, ↓ QT interval
Beta-receptor: Na+ (SA/AV)-block and Ca2+-block; negative chronotropic, dromotropic, and inotropic
Mg2+: Functional Ca2+ blocker; first line in Torsades de Pointes, Digitoxin toxicity
Adenosine: Receptors on SA and AV node; ↑ K+ and ↓ Ca2+ conductance, hyperpolarizes; may cause AV block; DOC in diagnosing/abolishing AV nodal arrhythmias. Toxicity: flushing, chest burning. t1/2 = 10s.
Hope it helps, topher.
http://rumorsweretrue.wordpress.com