This is a tricky situation.
Options include:
1. TRT yes, PCI (WBRT) yes
2. TRT yes, PCI (SRS) yes
3. TRT yes, PCI (WBRT/SRS) no
4. TRT no, PCI (WBRT) yes
5. TRT no, PCI (SRS) yes
6. TRT no, PCI (WBRT/SRS) no --> Observation
1. Would be what Slotman et al did. However: Patients in the Slotman trial were ineligible if they had brain metastasis at any point, although we do not know if the investigators checked for that at diagnosis (as was done in your patient) or at the point of randomization (after chemotherapy). If you had only checked after chemotherapy, you would have never known that your patient had a brain metastasis at presentation. Since the benefit of TRT was only visible at the 2-year-FU and the trial was negative for its primary endpoint, I think you can only argue to do this if you think your patient will truly benefit. Which means, you should tell us a bit more about him. Did he only have the one brain metastasis that made him ES or were there other mets too? If his liver was full of disease or he had multiple bone mets, I would be very reluctant to advocate for 1.
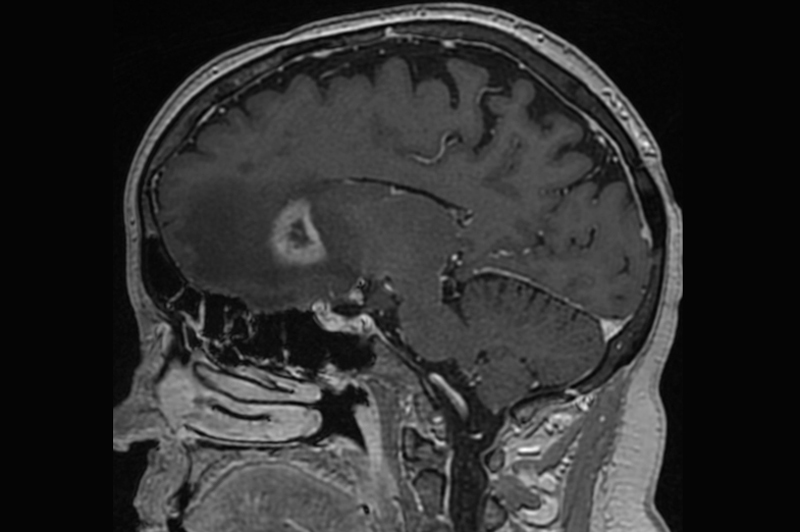
2. Not backed up by any evidence. SRS may be an option if there was residual disease in the brain, given he only had this 1 metastasis, but you could simply observe and treat when it reappears (if it reappears and the patient doesn't die of multilocular tumor progression in the mean time).
3. "If you are going to do TRT, you should do PCI too." Speaking from a "purist" point of view, that's the evidence, at least that's what Slotman did. On the other hand, I could personally live with such an approach, given that the only residual site of disease seems to be the chest right not and TRT will probably prolong PFS. Again, this approach is highly dependent on the initial extent of the disease outside the chest in other organs (apart from the brain). It's certainly a favorable approach in terms of limiting toxicity now, since you are skipping PCI.
4. It's what the original EORTC trial did, but that was all in the era of "no-MRI-done".
5. I wouldn't do it.
6. From a purist point of view that is correct. You do not have any data pointing at a survival benefit with PCI (it's not proplylactic anyway, since there was a macroscopic met in the beginning anyway!) if you have had brain metastasis and there is no known benefit of TRT in patients with documented brain metastases.
My recommendation:
Option 1 IF this was a patient with only a brain metastasis in the beginning, no other known extracerebral disease and not vastly advanced disease in the mediastinum (not bulky, multi nodal N2/N3). In fact, in such a scenario one could actually question if that is enough or if one should "go all in" and perform a
"Jeremic-like" approach with another couple cycles of cisplatinum/etoposide + full dose TRT + PCI going for a small, but perhaps possible, 10% chance of long-term cure.
Option 3 IF this was a patient with small / confined metastases outside of the thorax / brain at diagnosis. Not backed by any data, but appealing to me.
Option 6 IF this was a patient with considerable volume of metastases at diagnosis outside of the thorax & the brain