- Joined
- Jan 27, 2011
- Messages
- 292
- Reaction score
- 46
- Points
- 4,651
- Attending Physician
Advertisement - Members don't see this ad
Hello, I have a few questions about the above, and am hoping someone can help me out with their wisdom.
In young infants especially premature ones, they often come to us on fluids mixed with dextrose. I understand the need for dextrose in that population, but how does one calculate what solution to use? I've seen all types of Dextrose concentration mixed with all types of sodium concentration. When do I use d10/5 mixed with .45 saline or .225 saline etc? And how does this work? As the infant burns up the dextrose, aren't we essentially giving the baby a hypotonic solution? Why is this not harmful?
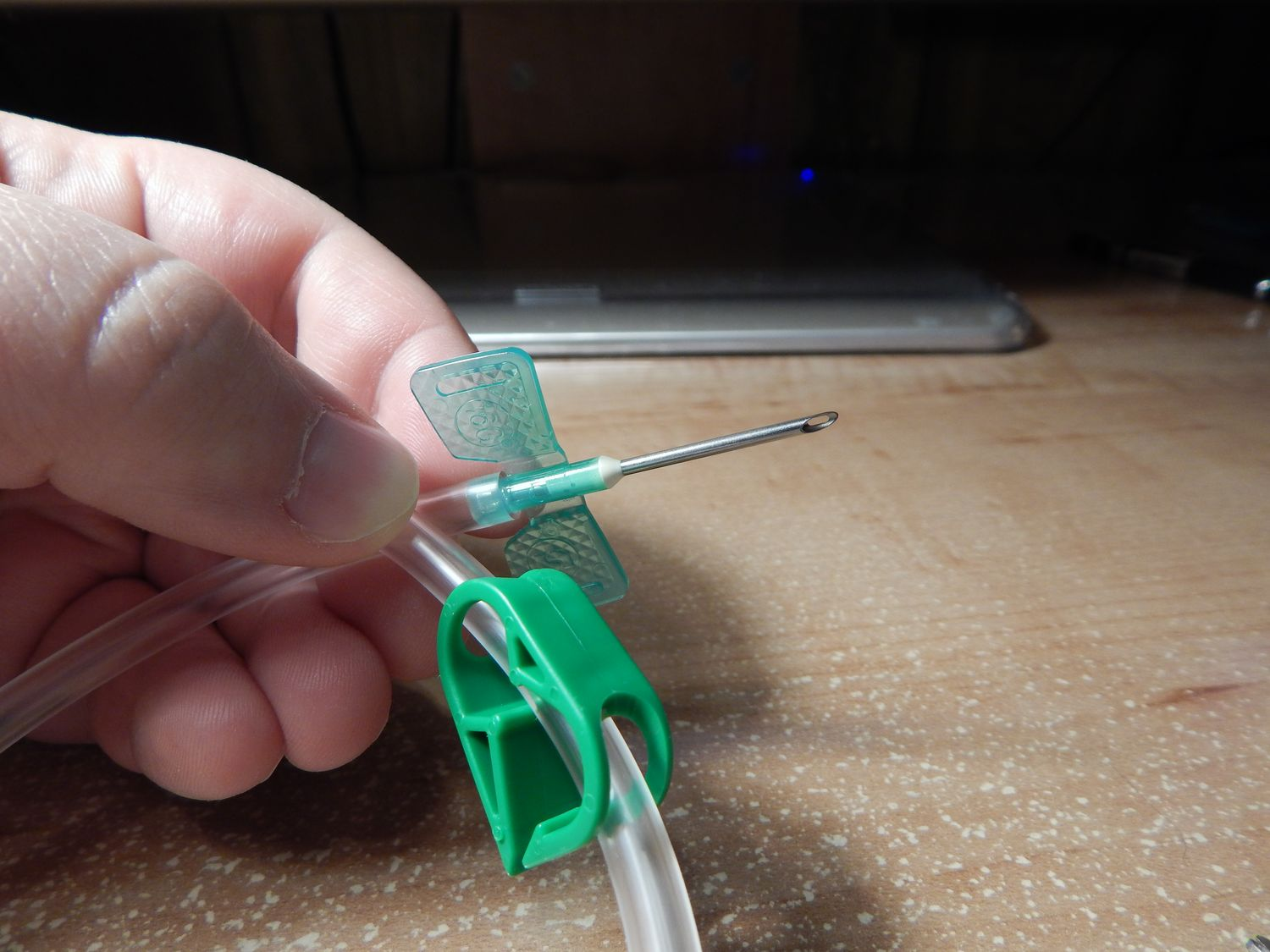
Another question is for ESRD patients with a fistula, is the main reason that we don't put IVs on that arm because the fistula may get infected? How do they use the fistula for dialysis? It confuses me why the arm can be used for dialysis but not for other things. I ask because there was a case with a complication that resulted in lots of blood loss. We were unable to get central access, the other arm had small veins so we could only put a couple small IVs. I was not allowed to touch the arm with the fistula because there's a fistula. Has anyone ever accessed the fistula for emergent access???
In young infants especially premature ones, they often come to us on fluids mixed with dextrose. I understand the need for dextrose in that population, but how does one calculate what solution to use? I've seen all types of Dextrose concentration mixed with all types of sodium concentration. When do I use d10/5 mixed with .45 saline or .225 saline etc? And how does this work? As the infant burns up the dextrose, aren't we essentially giving the baby a hypotonic solution? Why is this not harmful?
Another question is for ESRD patients with a fistula, is the main reason that we don't put IVs on that arm because the fistula may get infected? How do they use the fistula for dialysis? It confuses me why the arm can be used for dialysis but not for other things. I ask because there was a case with a complication that resulted in lots of blood loss. We were unable to get central access, the other arm had small veins so we could only put a couple small IVs. I was not allowed to touch the arm with the fistula because there's a fistula. Has anyone ever accessed the fistula for emergent access???