- Joined
- Oct 8, 2022
- Messages
- 132
- Reaction score
- 333
Hello,
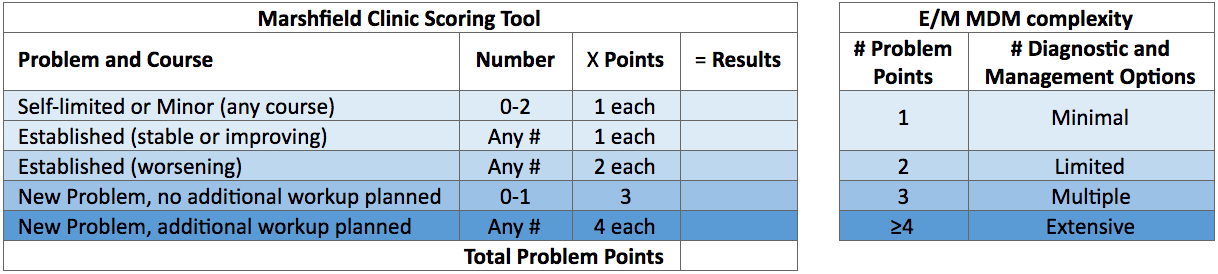
I am a new attending and have noticed some of my colleagues generate more RVUs per patient than I do in our monthly 'shame on you' meeting. I work on a nearly 100% RVU payscale. My understanding is a level 5 chart generates 4 RVUs and some of my colleagues average 5 RVUs or more per patient and we do not see that serious of acuity all the time. I do understand how to achieve a level 5 chart and requirements. I was wondering if anyone had some tricks or tips about how to generate more RVU's on top of the level 5 chart. I am also aware of when you can and can not bill for critical care time.
1) Does adding a differential to your note actually add RVUs? I had heard this in the past although for litigation I was told this is negative. For example, putting PE on a chest pain differential (in someone that PERC/WELLs out) and not acquiring a CTPE study.
2) Does writing that you reviewed 'old charts' increase RVUs?
3) Does a longer MDM create more RVU's? Mine are generally pretty short I am not sure if the private billing company will just see if I wrote 2 lines vs. 10 lines and determine complexity based of that
Appreciate the help!
I am a new attending and have noticed some of my colleagues generate more RVUs per patient than I do in our monthly 'shame on you' meeting. I work on a nearly 100% RVU payscale. My understanding is a level 5 chart generates 4 RVUs and some of my colleagues average 5 RVUs or more per patient and we do not see that serious of acuity all the time. I do understand how to achieve a level 5 chart and requirements. I was wondering if anyone had some tricks or tips about how to generate more RVU's on top of the level 5 chart. I am also aware of when you can and can not bill for critical care time.
1) Does adding a differential to your note actually add RVUs? I had heard this in the past although for litigation I was told this is negative. For example, putting PE on a chest pain differential (in someone that PERC/WELLs out) and not acquiring a CTPE study.
2) Does writing that you reviewed 'old charts' increase RVUs?
3) Does a longer MDM create more RVU's? Mine are generally pretty short I am not sure if the private billing company will just see if I wrote 2 lines vs. 10 lines and determine complexity based of that
Appreciate the help!