- Joined
- Sep 7, 2014
- Messages
- 3,206
- Reaction score
- 5,904
Which are people generally doing?
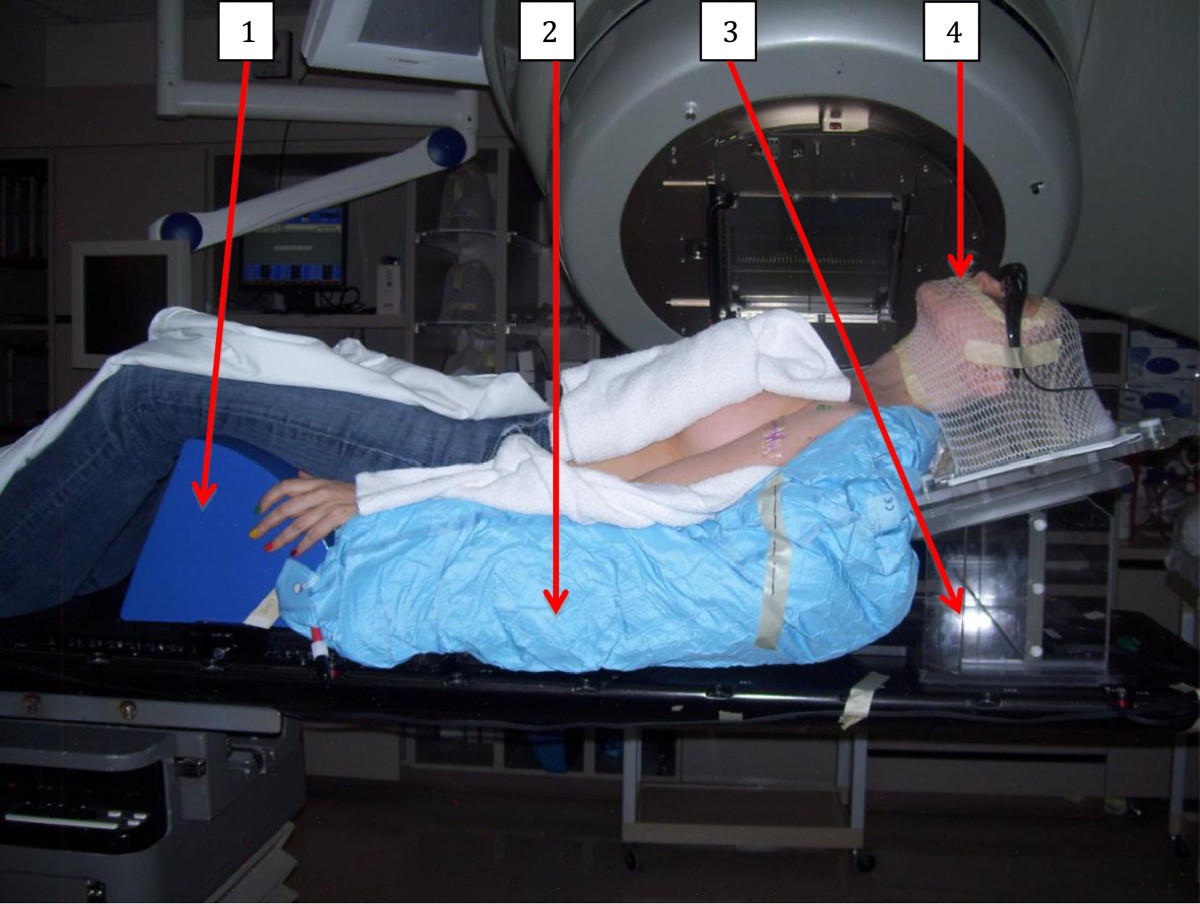
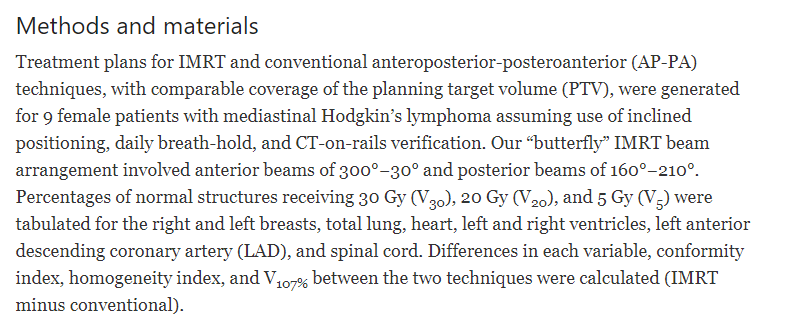
4dct? You dont wanna miss!More important than technique is the image guidance imo.. Daily CBCT, fast 3-4 hours before sim and daily treatment
right to the latter, just wondering if people are doing VMATMore important than technique is the image guidance imo.. Daily CBCT, fast 3-4 hours before sim and daily treatment. Can get a decent plan either way. Medicare will pay for IMRT if you think it looks better
More important than technique is the image guidance imo.. Daily CBCT, fast 3-4 hours before sim and daily treatment. Can get a decent plan either way. Medicare will pay for IMRT if you think it looks better
3D... been burned by IMRT a few times.
I would do a 4 field static beam IMRT plan and turn the smoothing up on each beam. I could just make a nicer bit more homogenous plan than what you guys are calling 3D. I would also call this IMRT approach 3D.Which are people generally doing?
Explain ? Curious to understand how I could screw this up3D... been burned by IMRT a few times.
I had one patient with MALT who had a distended stomach at baseline (I think some component of gastroperesis 2/2 diabetes) and, despite being NPO, his stomach volume was vacillate dramatically from day to day. I had originally planned him VMAT because his stomach was so large, we were starting to get into kidney territory... but I ended up switching him to 3D because the highly conformal VMAT plan was too tight some days on CBCT.Explain ? Curious to understand how I could screw this up
Let’s say the malt got 4 gy,( and there is nowExplain ? Curious to understand how I could screw this up
Doesn’t sound like a technique issue?I had one patient with MALT who had a distended stomach at baseline (I think some component of gastroperesis 2/2 diabetes) and, despite being NPO, his stomach volume was vacillate dramatically from day to day. I had originally planned him VMAT because his stomach was so large, we were starting to get into kidney territory... but I ended up switching him to 3D because the highly conformal VMAT plan was too tight some days on CBCT.
I mean... I could have thrown on a 2 cm margin and still done VMAT, but 3D worked just fine... just had to get creative with field arrangement. Sometimes a shotgun is better than a riffle (although, I don't have much experience with either haha)Doesn’t sound like a technique issue?
Motion is a problem always and 3D doesn’t fix that - you’re just using bigger margins, right?
That makes sense. I don’t know the gun analogy well!I mean... I could have thrown on a 2 cm margin and still done VMAT, but 3D worked just fine... just had to get creative with field arrangement. Sometimes a shotgun is better than a riffle (although, I don't have much experience with either haha)
right to the latter, just wondering if people are doing VMAT
close enough?If you ask ASTRO - there's only one answer.
PROTON.

Man.close enough?

Proton therapy in the management of non-Hodgkin lymphoma
Proton therapy (PT) is a highly conformal type of radiation therapy that can target the tumor while sparing dose to surrounding normal tissues. This study reviews a single institution's experience managing patients with non-Hodgkin lymphoma (NHL) treated ...www.ncbi.nlm.nih.gov
Triple or quadruple (the price of) therapyAh yes everyone knows that the initial medical management for gastric MALT involves a PPI -
PPS-exempt Proton Institution.
This wasn't a failure of modality but of margins (as you I'm sure know!); a preparation error and not an execution error.I had one patient with MALT who had a distended stomach at baseline (I think some component of gastroperesis 2/2 diabetes) and, despite being NPO, his stomach volume was vacillate dramatically from day to day. I had originally planned him VMAT because his stomach was so large, we were starting to get into kidney territory... but I ended up switching him to 3D because the highly conformal VMAT plan was too tight some days on CBCT.
You kill me with this @evilbooyaa ! You’re a young guy - how is it better ? Our faculty did a real number on us about the value of treatment technique.Agree w/ depends on anatomy, can do 3D or VMAT. 3D might be better if can stay off kidneys.
You kill me with this @evilbooyaa ! You’re a young guy - how is it better ? Our faculty did a real number on us about the value of treatment technique.
If the target is the same - which it should be - I’m curious as to what parameter would be better with 3D? If you did 4-5 static imrt fields, maybe V5 marginally better.
I think I just signaled Ryckman
IMO, you can do either and the potential to reduce “near misses” with 3D depends on how you do it. The stomach has a lot more degrees of freedom to move/rotate and distort than a lot of organs. If you use a 4-field box, you will have more wiggle room in at least some directions than with IMRT. Are they the right directions? Not a guarantee but there will be more wiggle room. Now if you use more fields and get super conformal…not so much. Might as well do VMAT and make it a fast delivery.You kill me with this @evilbooyaa ! You’re a young guy - how is it better ? Our faculty did a real number on us about the value of treatment technique.
If the target is the same - which it should be - I’m curious as to what parameter would be better with 3D? If you did 4-5 static imrt fields, maybe V5 marginally better.
I think I just signaled Ryckman
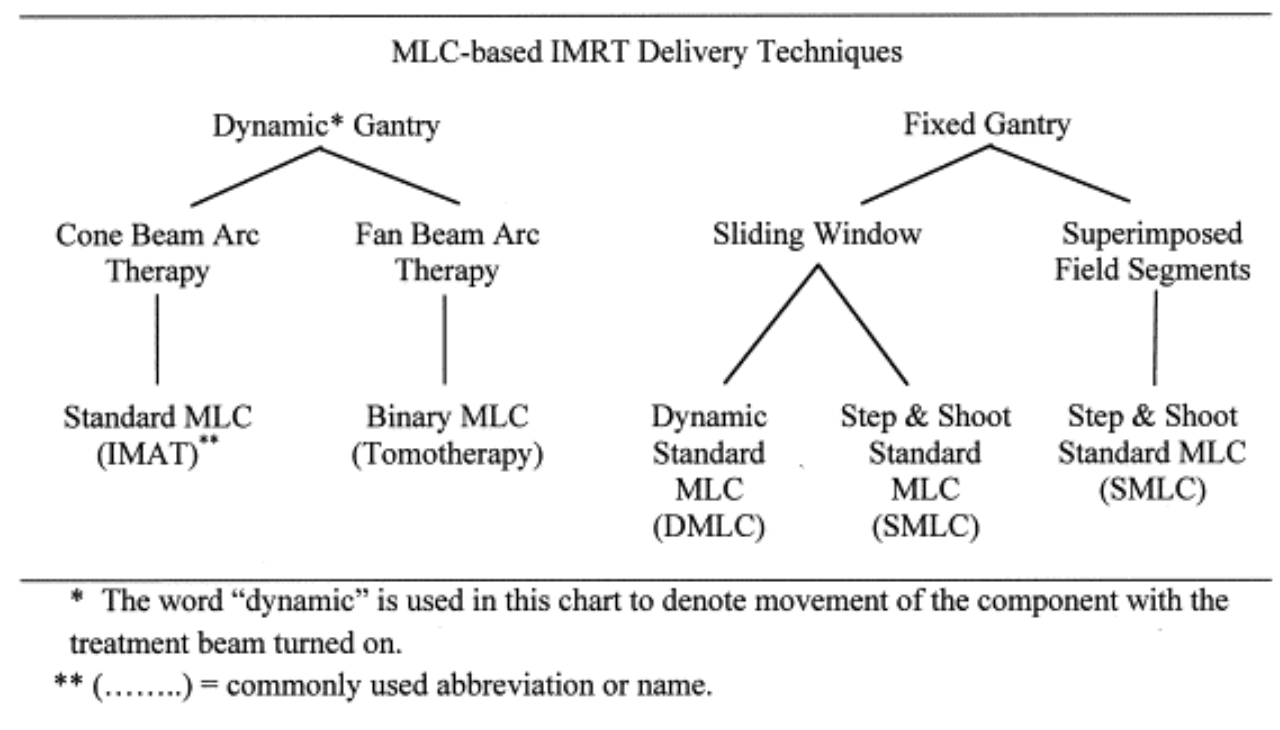
VMAT is a type of IMRT3D might be better than VMAT is what I said. As I'm sure you're aware, static IMRT != VMAT. VMAT will likely lead to higher kidney doses than 3D. I do not routinely using static IMRT in 2022 because if I'm doing 3D I'm usually getting a good homogeneous plan, which is the main thing static IMRT can improve upon (same concept as sliding window) that I am comfortable with.
If I feel like I can get decent homogeneity with a 3 or 4-field box w/ 3D why would I bother with static IMRT? Especially for 30Gy? When the main reason patients get symptoms is due to radiation of the target itself (the stomach)? 3D can have a treatment that takes a shorter amount of time to deliver with an otherwise functionally equivalent plan.
Also, static IMRT is not the same as sliding window and the goal of it is not generally yo improve homogeneity. How do you think we did IMRT for everything way back when? 5,7,9 static fields to create concave shaped fields.That’s reasonable. But I don’t think I’ve ever seen better dosimetry in the abdomen.
VMAT is a type of IMRT
Like saying radiation does not equal protons.
At the risk of going full Scarb, I get it. I’m a stickler for the fact that basically it’s all just manipulation of fluence and the target is the target is the target.
ESE/Scarb - dose cloud , probabilities , blah blah blah
Ha! I’d love to see your Press-Gainey scores.
Is field-in-field IMRT? Lol sorry, couldn’t miss a chance to trollThat’s reasonable. But I don’t think I’ve ever seen better dosimetry in the abdomen.
VMAT is a type of IMRT
Like saying radiation does not equal protons.
At the risk of going full Scarb, I get it. I’m a stickler for the fact that basically it’s all just manipulation of fluence and the target is the target is the target.
ESE/Scarb - dose cloud , probabilities , blah blah blah
Man….Is field-in-field IMRT? Lol sorry, couldn’t miss a chance to troll
That’s reasonable. But I don’t think I’ve ever seen better dosimetry in the abdomen.
VMAT is a type of IMRT
Like saying radiation does not equal protons.
At the risk of going full Scarb, I get it. I’m a stickler for the fact that basically it’s all just manipulation of fluence and the target is the target is the target.
ESE/Scarb - dose cloud , probabilities , blah blah blah
Huh???As I'm sure you're aware, static IMRT != VMAT.
If you use a 4-field box, you will have more wiggle room in at least some directions than with IMRT.
Same as a resident, and I can only hope to pass that along to future generations, with the goal being to educate without as much of the raised eye-brows semantics discussion (understanding that meanings of words change over time to fall into line with local colloquialisms, AKA hotspot) that plagues a few of the regulars. There were a few of the original zombies, others have been more recently infected.I've learned more about tx planning and dosimetry on SDN than I did in residency.
I feel like you are mocking meThere should be a 4 field box option in arc planning as this is totally achievable and probably quicker to plan and prettier, and qa these days using portal dosimetry is probably quicker than shooting 4 ports. Then everyone can be happy
There should be a 4 field box option in arc planning as this is totally achievable and probably quicker to plan and prettier, and qa these days using portal dosimetry is probably quicker than shooting 4 ports. Then everyone can be happy

Kinda joking. Can open the leaves from 358 to 2 degrees, 88-92 degrees, 178-182 degrees, and 268-272 degrees. Would be a nice "4 field box."
there is something about the hardware engineering that the gantry would have to move so slowly to "spray" the fluences over just a 178-182 degree travel (also, isn't this an impossible arc, because the gantry can't slide past about 181 on the downward side, at least on a Varian machine... ethos and halcyon may be different idk if they are "slip gantries") that something doesn't work mechanically. I think the thing I'm thinking of is... MUs per degree??? Too many MUs per degree with short-angle arcs? Anyways, the minimum arc is usually 30 degrees from start angle to stop angle: to wit, your link...Kinda joking. Can open the leaves from 358 to 2 degrees, 88-92 degrees, 178-182 degrees, and 268-272 degrees. Would be a nice "4 field box."
Like this version of AP/PA
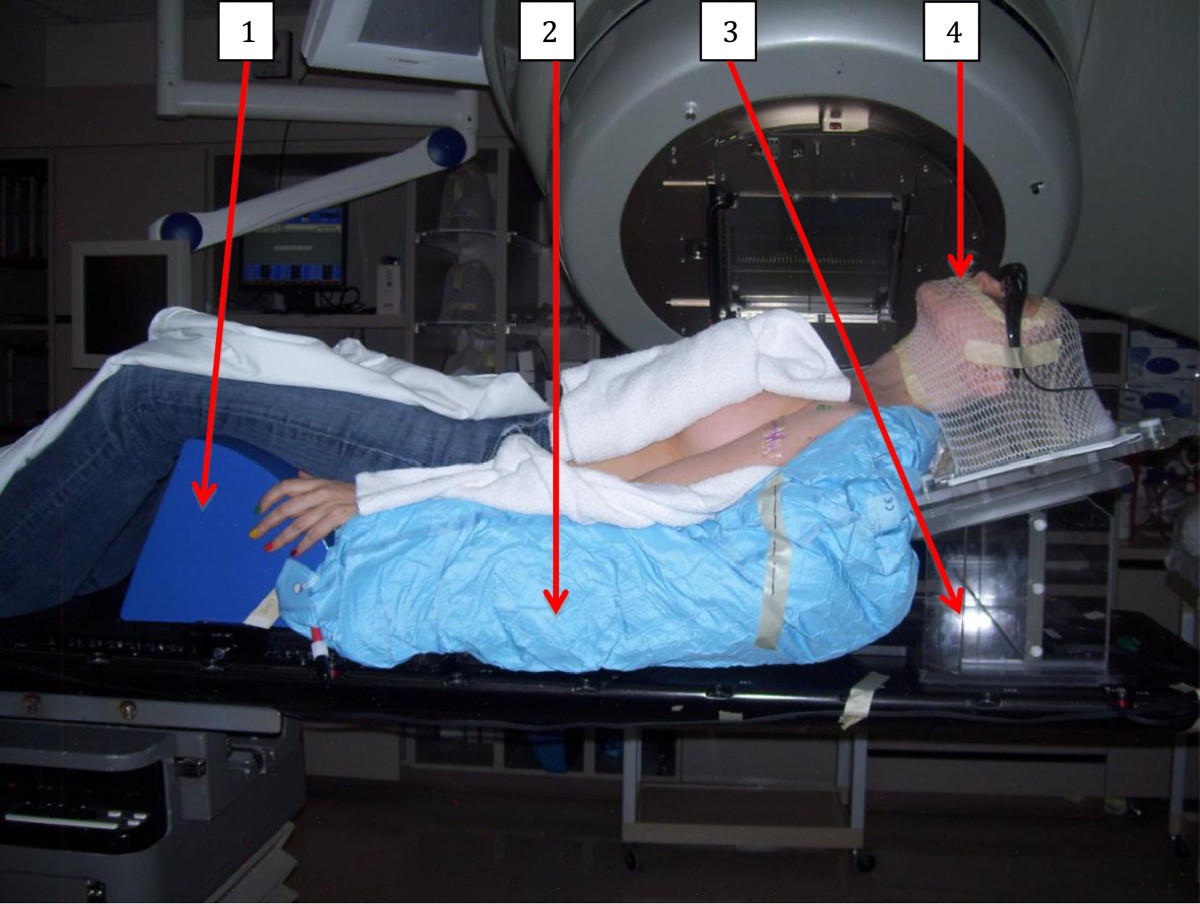
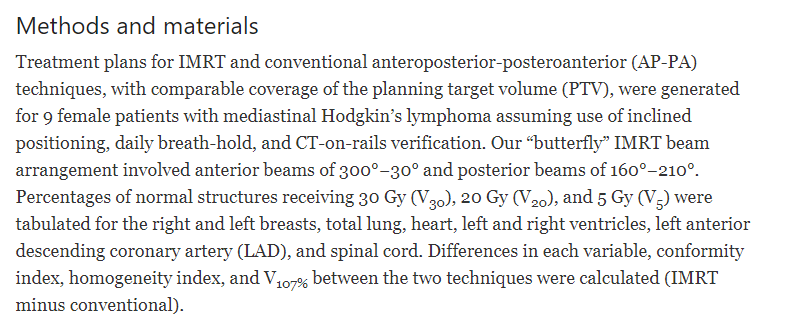
Dosimetric advantages of a “butterfly” technique for intensity-modulated radiation therapy for young female patients with mediastinal Hodgkin’s lymphoma - Radiation Oncology
Purpose High cure rates for Hodgkin’s lymphoma must be balanced with long-term treatment-related toxicity. Here we report an intensity-modulated radiation therapy (IMRT) technique that achieves adequate target coverage for mediastinal disease while minimizing high- and low-dose exposure of...ro-journal.biomedcentral.com
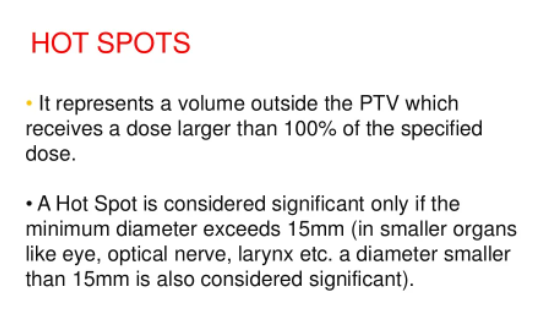
By definition it is not a hot spot.Thinking hot spot is a problem to say is part of the problem! That’s a made up semantic rule
It is a hot spot! The difference is with SBRT we want hot spots and with standard VMAT people don’t like them (and they should be fine with hot spots, that’s a boomer vestige to not want hot spots in a chemoRT plan IMO) but it absolutely is by definition a hot spot.
I can never remember where they start, but if so, 180-78 and then 182-180 or therabout. I didn't say we yet possess the tech to entirely recreate a 4 field box in a single arc, but this doesn't sound hard. It's worth finding out.there is something about the hardware engineering that the gantry would have to move so slowly to "spray" the fluences over just a 178-182 degree travel (also, isn't this an impossible arc, because the gantry can't slide past about 181 on the downward side, at least on a Varian machine... ethos and halcyon may be different idk if they are "slip gantries") that something doesn't work mechanically. I think the thing I'm thinking of is... MUs per degree??? Too many MUs per degree with short-angle arcs? Anyways, the minimum arc is usually 30 degrees from start angle to stop angle: to wit, your link...