I have this patient with atypical facial pain / ? Trigeminal neuralgia refractory to med mgmt( carbamazepine, gabapentin, topomax), 2 gamma knife procedures ( with 2 month relief) . Pain is continuous, stabbing, sharp pain, paresthesisas on rt side of the face. Initially pain was supra and infra orbital radiating to towards rt ear now he started pain in gums. Options I am considering are supra and infra orbital nerve blocks/ Stellate ganglion block/ Sphenopalatine ganglion blocks/ gasserian ganglion block/ occipital / peripheral nerve stimulators. Any thoughts ?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
interventional options for Trigeminal neuralgia
- Thread starter painfre
- Start date
- Joined
- Sep 22, 2006
- Messages
- 167
- Reaction score
- 2
I'm helping my attending (I'm a CA 2)place a permanent peripheral nerve stim for trigeminal neuralgia tomorrow. The trial decreased the patient's pain by 75 %. This is the 6 th peripheral stim he has placed over the last about 6 months for trigeminal neuralgia.
- Joined
- May 30, 2005
- Messages
- 21,253
- Reaction score
- 12,367
1. Meds: trial of Trileptal. Amazing results for folks who have failed other meds. No idea why- but I have 5 patients of so who it is working well for.
2. SPG with sterile applicator to posterior nasopharynx. 2% lidocaine in syringe. See WIndsor's article or search the forum for how to assemble an inexpensive system for delivering the med to the nasopharynx and not just down the nose.
3. Gasserian- Way Yin article on how to get it done. Local only for the first one and if there is relief I will repeat and pulse it. Too chicken to RF the bugger because the eyeball can dry out and die.
4. PNS: works great for 6 months. Have seen leads erode through skin, migration issues, and no one I've seen has had relief passed one year. Pain will find a way. If you implant, send them to me next year because I collect batteries from other people's mistakes. Also, from an insurance standpoint- it will always be experimental/investigational. I know it won't stop anyone from trying, but it will end in failure.
Still looking for local folks in Georgia who don't mind burning the G-spot- but I won't do it.
Get them involved in psychology/counseling- this was 50% fatal due to suicide 100 years ago.
2. SPG with sterile applicator to posterior nasopharynx. 2% lidocaine in syringe. See WIndsor's article or search the forum for how to assemble an inexpensive system for delivering the med to the nasopharynx and not just down the nose.
3. Gasserian- Way Yin article on how to get it done. Local only for the first one and if there is relief I will repeat and pulse it. Too chicken to RF the bugger because the eyeball can dry out and die.
4. PNS: works great for 6 months. Have seen leads erode through skin, migration issues, and no one I've seen has had relief passed one year. Pain will find a way. If you implant, send them to me next year because I collect batteries from other people's mistakes. Also, from an insurance standpoint- it will always be experimental/investigational. I know it won't stop anyone from trying, but it will end in failure.
Still looking for local folks in Georgia who don't mind burning the G-spot- but I won't do it.
Get them involved in psychology/counseling- this was 50% fatal due to suicide 100 years ago.
- Joined
- Aug 15, 2007
- Messages
- 1,426
- Reaction score
- 542
pRF ok for Atypical Trigeminal pain. Would not do tRF secondary to, in my clinical experience, showing little efficacy for the constant component.
tRF shows very high efficacy for class Tic!
tRF shows very high efficacy for class Tic!
- Joined
- Jul 26, 2010
- Messages
- 2,348
- Reaction score
- 197
I assume that you already consulted psych etc....agree it's important in this population.
IN terms of interventions. Which distribution is it in? If it's in V1, likely will have to do a gasserian. If it's V2/v3, you might be able to get away with a trans coronoid approach, but you wont get V1.
You can pulse the gasserian, I think Sluitjer has some articles on it...problem is getting paid.
IF you can anchor the peripheral stim nicely, it's an option I've seen done. They talked about this actually at ASRA this past year. guys like narouze were doing it.
IN terms of interventions. Which distribution is it in? If it's in V1, likely will have to do a gasserian. If it's V2/v3, you might be able to get away with a trans coronoid approach, but you wont get V1.
You can pulse the gasserian, I think Sluitjer has some articles on it...problem is getting paid.
IF you can anchor the peripheral stim nicely, it's an option I've seen done. They talked about this actually at ASRA this past year. guys like narouze were doing it.
- Joined
- Oct 3, 2007
- Messages
- 300
- Reaction score
- 1
in addition to carbamazepine (you can increase dose until side effects occur, similar to neurontin. one patient up to 2000/day i saw in neurology ha clinic)
also trigeminal ganglion pulse or rf, and facial stim leads which work well, consider a trigeminal ganglion stimulator lead placed into the foramen.
seen 2, good results. just a thought
also trigeminal ganglion pulse or rf, and facial stim leads which work well, consider a trigeminal ganglion stimulator lead placed into the foramen.
seen 2, good results. just a thought
- Joined
- Apr 23, 2006
- Messages
- 369
- Reaction score
- 74
I do thermal RF on Gasserians - about 5 per year. V2 and 3 respond well, V1 not so much. 60 degress for 80 seconds. About 1 in 4 patients needs a re-burn at 80 for 80. No dolorosa, corneal anesthesia. The success rate is excellent, and it is very safe. I do under GA because usually these patients have been habituated to anti-seizure meds and are hard to sedate with just Versed.
For V1 or more atypical presentations, I have found Botox quite effective. Not really worth trying to get insurance coverage, just charge $9 per unit, 25 units or less usually.
For V1 or more atypical presentations, I have found Botox quite effective. Not really worth trying to get insurance coverage, just charge $9 per unit, 25 units or less usually.
- Joined
- Oct 23, 2005
- Messages
- 813
- Reaction score
- 10
Botox subQ or on the nerve?
- Joined
- May 30, 2005
- Messages
- 21,253
- Reaction score
- 12,367
I do thermal RF on Gasserians - about 5 per year. V2 and 3 respond well, V1 not so much. 60 degress for 80 seconds. About 1 in 4 patients needs a re-burn at 80 for 80. No dolorosa, corneal anesthesia. The success rate is excellent, and it is very safe. I do under GA because usually these patients have been habituated to anti-seizure meds and are hard to sedate with just Versed.
For V1 or more atypical presentations, I have found Botox quite effective. Not really worth trying to get insurance coverage, just charge $9 per unit, 25 units or less usually.
Excellent. If my folks get less than 3 months with pulsed, I can send them up the road for a burning?
- Joined
- Mar 30, 2003
- Messages
- 3,113
- Reaction score
- 880
I took my mom to see Ben Carson last year to discuss options for treating her TN (back in remission, for now). His first choice for all but young patients is glycerol rhizotomy. Generally it can be repeated a few times before scar tissue becomes a problem. If it does, he uses RF to zap the scar tissue, and then do another glycerol rhizotomy. I didn't ask for the details on how he knows he's only killing scar tissue with the RF, but he's Ben Carson.. so I'm sure there's some magic involved.
He was on the fence about offering my mom a MVD, as she's 73 and has lupus (but no CV, pulm, or renal comorbidities). My grandparents on her side died at 88 and 93, so she could certainly live another 10-15 years, thus MVD is a serious consideration. Having said that.. who's comfortable having their mom's head opened up? She's in remission now, so we have some time to think about it.
He was on the fence about offering my mom a MVD, as she's 73 and has lupus (but no CV, pulm, or renal comorbidities). My grandparents on her side died at 88 and 93, so she could certainly live another 10-15 years, thus MVD is a serious consideration. Having said that.. who's comfortable having their mom's head opened up? She's in remission now, so we have some time to think about it.
- Joined
- Apr 23, 2006
- Messages
- 369
- Reaction score
- 74
Sam Hassenbusch taught me how to do these while was a fellow with Allen Burton. Did about 10 in fellowship and about 20 since then. Steve, it would be an honor to care for one of your patients. I would choose RF for myself over MVD any day.
For botox, SQ injections in the area of pain. Supposedly there is uptake all the way to the ganglion. Same as in migraine. Definitely better for atypical facial pain than neurodestruction.
For botox, SQ injections in the area of pain. Supposedly there is uptake all the way to the ganglion. Same as in migraine. Definitely better for atypical facial pain than neurodestruction.
- Joined
- Aug 15, 2007
- Messages
- 1,426
- Reaction score
- 542
I do thermal RF on Gasserians - about 5 per year. V2 and 3 respond well, V1 not so much. 60 degress for 80 seconds. About 1 in 4 patients needs a re-burn at 80 for 80. No dolorosa, corneal anesthesia. The success rate is excellent, and it is very safe. I do under GA because usually these patients have been habituated to anti-seizure meds and are hard to sedate with just Versed.
For V1 or more atypical presentations, I have found Botox quite effective. Not really worth trying to get insurance coverage, just charge $9 per unit, 25 units or less usually.
GA, how do you know which division you are on w/o sensory stim? I use propofol and a little fentanyl. Wake them up, then query, put them back under and then lesion usually x 3. Thermal at 60, 65 and then 70 C. It takes about 45 minutes to 1 hour.
V1 RF also very effective, however, as you know you may lose corneal reflex. For the patients that wear glasses, not so much of a problem. However, I have found that if you use 60 seconds for burns, the corneals are usually only diminished and not lost.
Bringing back an old thread. I recently saw a female in her late twenties for right sided TN. Diagnosed 3 years ago and underwent Cyber Knife for it 2 years ago. Ever since then she has right sided facial numbness in V1-V3 with severe pain, tightness and eye watering. Brain MRI normal before the procedure. No vascular loops or other compressive lesions. Failing trileptal and gabapentin. I’ve never actually seen anesthesia dolorosa from trigeminal nerve ablation in person. I’ve only read about it. I do gasserian ganglion blocks and pulsed RF (cash pay) but not RFA. What can I offer this poor patient? I offered her a gasserian block to see if that could help but her insurance considers it experimental. SCS? Refer for DBS? Stellate? I’ve already told her there is likely no cure for it.
- Joined
- May 30, 2005
- Messages
- 21,253
- Reaction score
- 12,367
Trileptal 150 bid and baclofen 10 bid.
RFA is standard of care.
3 division pain is not organic. Maybe some overlap. Burn V2 and see what you get.
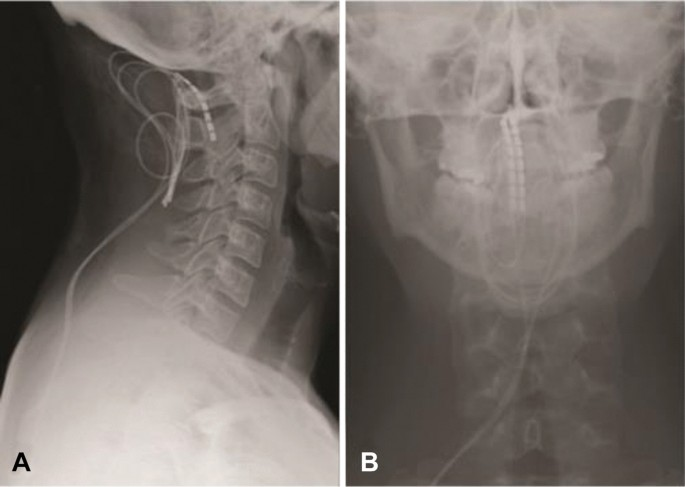
SCS at C2 can get V3 100% and V2 80% and V1 0% of the time. Coverage is no guarantee of relief.
RFA is standard of care.
3 division pain is not organic. Maybe some overlap. Burn V2 and see what you get.
SCS at C2 can get V3 100% and V2 80% and V1 0% of the time. Coverage is no guarantee of relief.
- Joined
- Oct 28, 2009
- Messages
- 629
- Reaction score
- 417
amitriptyline, topiramate, lyrica, duloxetine, and like 1/2 dozen other medications I would consider before DBS/Stellate/SCS
- Joined
- Jan 26, 2017
- Messages
- 54
- Reaction score
- 43
Steve,Trileptal 150 bid and baclofen 10 bid.
RFA is standard of care.
3 division pain is not organic. Maybe some overlap. Burn V2 and see what you get.
SCS at C2 can get V3 100% and V2 80% and V1 0% of the time. Coverage is no guarantee of relief.
Thanks for your input again. C2 Stim mechanism mediated through trigemino-cervical nucleus?
- Joined
- May 30, 2005
- Messages
- 21,253
- Reaction score
- 12,367
Nothing makes less sense than putting a cranial nerve nuclei at C2 inside the spinal cord. Is the only cranial nerve nuclei that does not exist inside the skull for protection. It is the ideal target.Steve,
Thanks for your input again. C2 Stim mechanism mediated through trigemino-cervical nucleus?
- Joined
- Dec 13, 2005
- Messages
- 5,316
- Reaction score
- 3,596
Trileptal. Nothing else works very well
Thanks for the responses. The patient has been on trileptal for several months as well as gabapentin without relief. She developed anesthesia dolorosa from her cyber knife procedure so i doubt she would pursue RFA of the Gasserian branches. Other than continued trials of neuropathics, in this case a stellate seems reasonable given her current condition and perhaps a cervical SCS trial based on the response? It seems her overall options are poor though.
There's a bunch of drugs to try. Lately I've been on a phenytoin kick, but Trileptal is first line for sure. I get that dose up a lot higher, topping out in the 1200 -1800 mg/day range.
The C2 stim is great. There are some retrograde C1-2 SCS cases that you could get a neurosurgeon to try perhaps before the DBS.
I would offer a SPG as she has autonomic changes. I like the suprazygomatic PPF approach out of UF

 www.ncbi.nlm.nih.gov
www.ncbi.nlm.nih.gov
A stellate is fine but you're really wanting the higher cervical sympathetic chain, which you'll get with a moderate to high volume SGB at C6, but you could also get better with the superficial block at C3-4.
Safety and utility of ultrasound-guided superior cervical ganglion block for headaches and orofacial pain: a retrospective, single-center study of 10 patients
The C2 stim is great. There are some retrograde C1-2 SCS cases that you could get a neurosurgeon to try perhaps before the DBS.
I would offer a SPG as she has autonomic changes. I like the suprazygomatic PPF approach out of UF

Ultrasound-Guided Suprazygomatic Nerve Blocks to the Pterygopalatine Fossa: A Safe Procedure
Large-scale procedural safety data on pterygopalatine fossa nerve blocks (PPFBs) performed via a suprazygomatic, ultrasound-guided approach are lacking, leading to hesitancy surrounding this technique. The aim of this study was to characterize the safety ...
A stellate is fine but you're really wanting the higher cervical sympathetic chain, which you'll get with a moderate to high volume SGB at C6, but you could also get better with the superficial block at C3-4.
Safety and utility of ultrasound-guided superior cervical ganglion block for headaches and orofacial pain: a retrospective, single-center study of 10 patients
painfreeasea
New Member
- Joined
- Dec 1, 2023
- Messages
- 1
- Reaction score
- 2
Hi...Bringing back an old thread. I recently saw a female in her late twenties for right sided TN. Diagnosed 3 years ago and underwent Cyber Knife for it 2 years ago. Ever since then she has right sided facial numbness in V1-V3 with severe pain, tightness and eye watering. Brain MRI normal before the procedure. No vascular loops or other compressive lesions. Failing trileptal and gabapentin. I’ve never actually seen anesthesia dolorosa from trigeminal nerve ablation in person. I’ve only read about it. I do gasserian ganglion blocks and pulsed RF (cash pay) but not RFA. What can I offer this poor patient? I offered her a gasserian block to see if that could help but her insurance considers it experimental. SCS? Refer for DBS? Stellate? I’ve already told her there is likely no cure for it.
I suggest that don't do any intervention for Anesthesia Dolorosa... don't have experiece of SCS for this indication though... but no RF etc. have seeen atleast 10 post- gamma/ cyber knife patients with Anesthesia Dolorosa, dont know why the incidence is so high..
