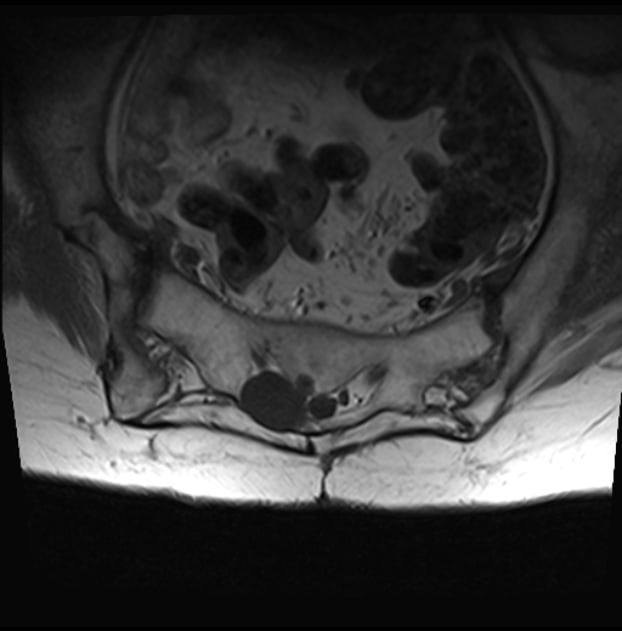
A lost battle with my arch nemesis the SI joint today. Very petite 82 year old with osteoporosis s/p L4-S1 PLIF with transitional anatomy manifesting as lumbarized S1. Old fashioned right side iliac crest bone graft harvest scar. Right buttock pain. Weight bearing LS spine x-ray showing right SIJ and axial MRI image showing only cross sectional view of SIJ. On fluoro straight AP there was what looked to be a long radiolucent “stripe”. The remainder of the sacrum was just a gray ground glass pattern. I tried to access the lower pole and middle. Each time after contrast injection there was a vascular pattern. I tried to oblique the image and separate that anterior and posterior joint surfaces but I could not establish the cortical margins of the joint. I tried the “Benyamin technique” where you tilt the II caudal and add some contralateral oblique to form a lucency where the joint lines cross in the middle. I couldn’t see any lucency but drove the needle where the joint lines appeared to cross. Felt like it entered the joint but all I got was a vascular pattern. After 25 minutes I just gave up. If our IR guy would do it I would send her for CT guidance. He won’t do anything MSK.
I’ve had this happen before in the elderly with osteoporosis. I can’t distinguish the tactile sensation of entry into the joint from entry into the soft bone.
Anyone have suggestions for this kind of situation? Any value to getting a CT and trying again with a better cross sectional view?

I’ve had this happen before in the elderly with osteoporosis. I can’t distinguish the tactile sensation of entry into the joint from entry into the soft bone.
Anyone have suggestions for this kind of situation? Any value to getting a CT and trying again with a better cross sectional view?