- Joined
- Jan 26, 2017
- Messages
- 87
- Reaction score
- 218
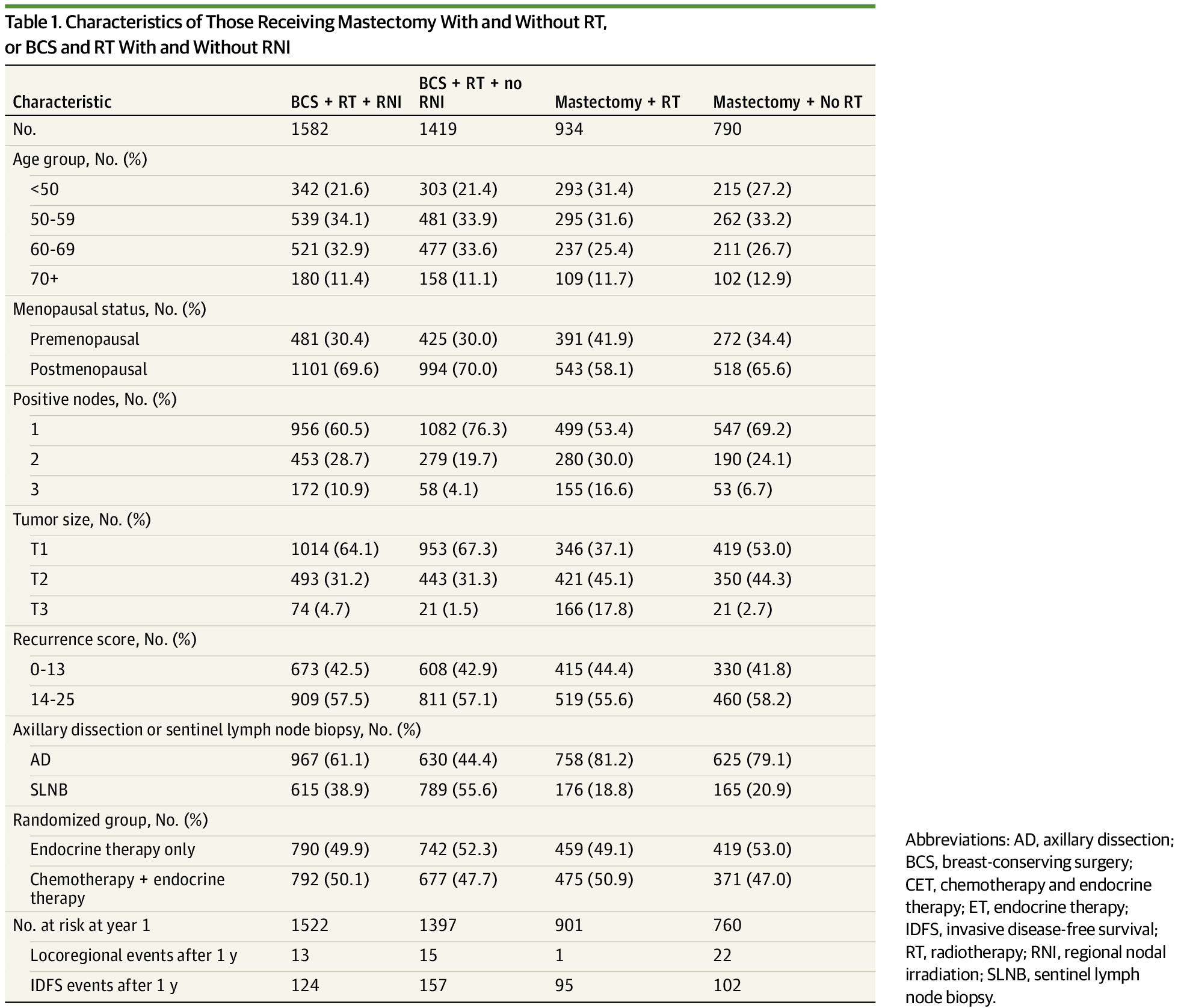
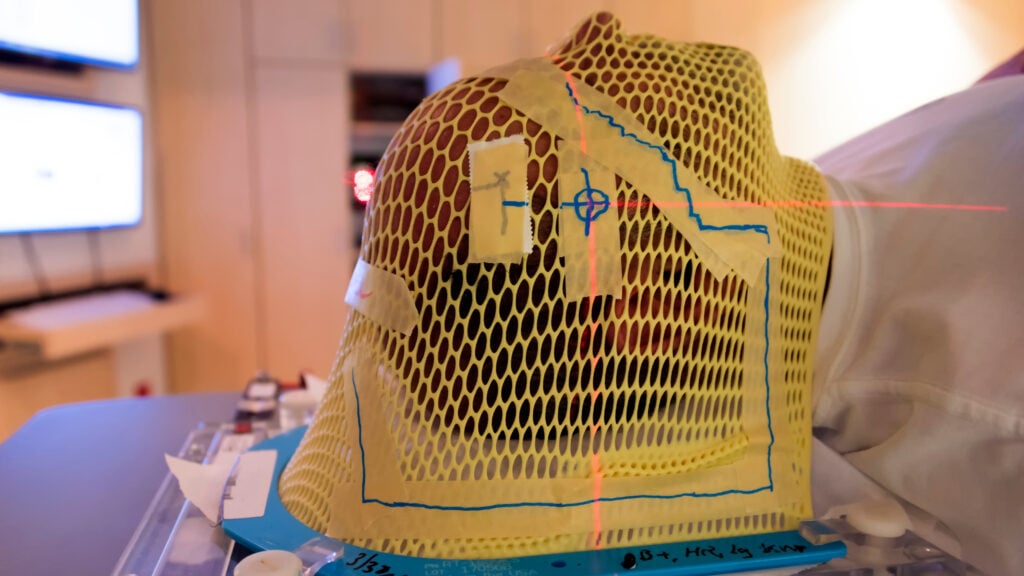
LUMINA in this weeks NEJM:All while articles like this are being published:
Radiation, a mainstay of cancer treatment, begins a fade-out
Radiation, a mainstay of cancer treatment, begins a fade-out
“There are situations now on an individual patient basis where radiation may not be needed.”www.statnews.com
Omitting Radiotherapy after Breast-Conserving Surgery in Luminal A Breast Cancer
Prepare for the subsequent clickbait (for example):
Some early-stage, low-risk breast cancer patients may not need radiotherapy after surgery

Some early-stage, low-risk breast cancer patients may not need radiotherapy after surgery
Some women with early-stage, low-risk breast cancer may not need radiotherapy after breast conserving surgery according to new research led by McMaster University, BC Cancer, Hamilton Heath Sciences, and the University of British Columbia.
Is it time to buy the dip?