- Joined
- Mar 22, 2008
- Messages
- 3,541
- Reaction score
- 2,163
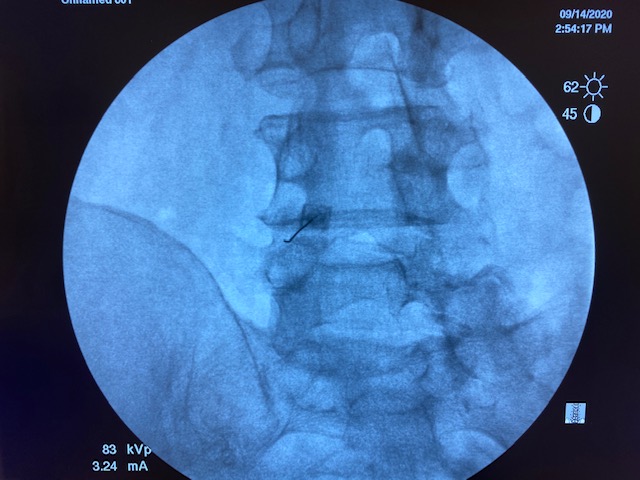
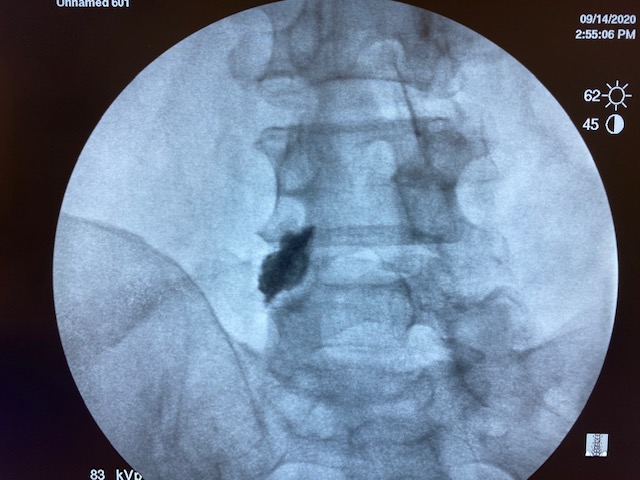
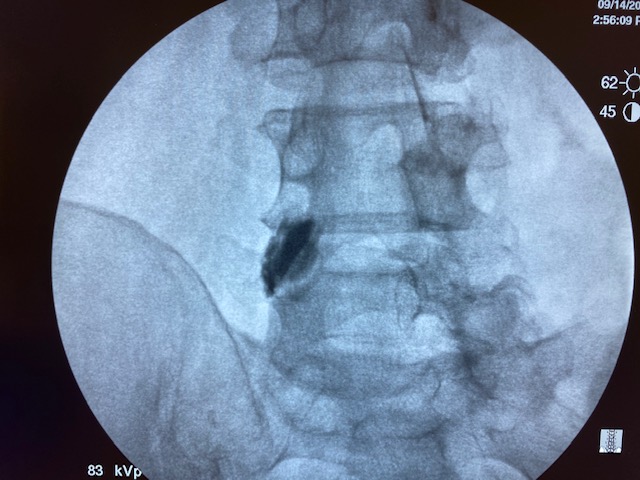
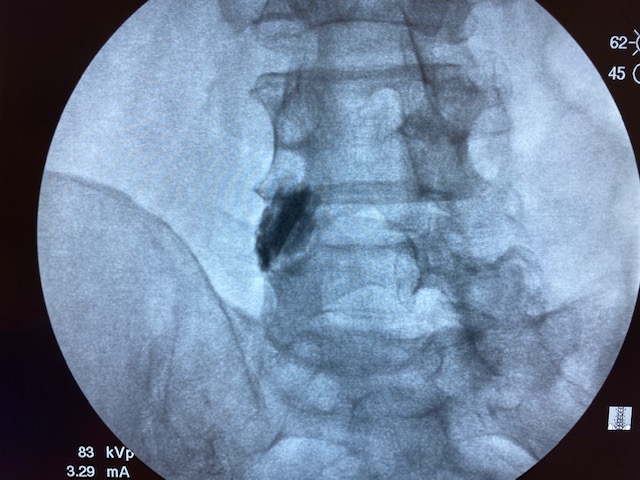
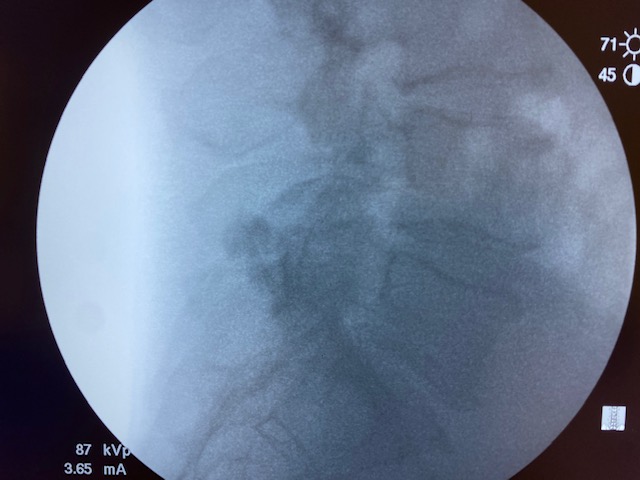
Literature says over 0.3cc is non-selective. But I've done this little experiment with my medical students multiple times. 1cc of contrast/local stays put. Each picture is 30 seconds apart.


Wat does the rfa have to do with this?Yep, 1ml is fine. I just do 1ml of 1% lido before RFA as well.
When I inject someone I have them get up and move right then. If I leave an adjacent level out, they know it even 5-10 minutes later. Block the adjacent level and the result changes. This technique appears to provide the same result than when I use SIS technique.1ml is not fine. Contrast spread on your table is not the same as spread of the anesthetic when patients get up and move around. How do you think SIS developed the guidelines?
When I inject someone I have them get up and move right then. If I leave an adjacent level out, they know it even 5-10 minutes later. Block the adjacent level and the result changes. This technique appears to provide the same result than when I use SIS technique.
What different methods for blocks have you investigated yourself over the years?
You know, this is an interesting question I've thought about in the past.
I usually do 0.5 - 0.75 cc per MBB needle. If I did higher volume, what is the structure I've anesthetized that confers a false positive block?
Do your med students understand wat ur doing and whyI’ve done this maybe 10-15 times to show my med students. It’s always the same with 1cc. 2cc travels to an adjacent level.
I have the SIS Guideline book there for them. These are kids going into fields other than this usually. It’s more to make the point to think critically and be reasonable investigators.Do your med students understand wat ur doing and why
I’ve done this maybe 10-15 times to show my med students. It’s always the same with 1cc. 2cc travels to an adjacent level.
How many trials of this did you do? That’s a nice little blob you’ve got there but the contrast spread is often no so neat and tidy. More pertinent to actual practice and not academic papers is that Medicare considers a valid MBB to be 0.5 mL or less so if you get audited and all your op reports show 1mL at each site for your MBBs, they could potentially rake back all your RF payments.
I'll do 5, 10, 15 minutes next time. That's more than enough for me personally. If you hurt with motion before the shot and can move fully after, I'm moving to RF.you'd have to flouro them an hour out, then 2, then 3 then 4 then 5. i dont think you'd even see the contrast after that long, but im not sure.
I'll do 5, 10, 15 minutes next time. That's more than enough for me personally. If you hurt with motion before the shot and can move fully after, I'm moving to RF.
Do you do anesthetize the skin and/or soft tissue? Think you'll get a ton of false positives with that criteria.
I'll do 5, 10, 15 minutes next time. That's more than enough for me personally. If you hurt with motion before the shot and can move fully after, I'm moving to RF.
I see two schools of thought. You can place your needle in the vicinity of the medial branch as seen on a 15-20 degree oblique view without your superior endplate parallel to the x-ray beam, inject 1 ml of contrast followed by 1ml LA. You will have more false positives and more failed RFN. In exchange you will have a lot less radiation exposure, move quicker and have more RFN billed out. On the opposite end you can make certain endplate is square, check a declined view and make certain your needle tip is in the SAP/TP sulcus and then get away with 0.3 ml of contrast and LA. In exchange you get a lot more radiation exposure, and less RFN billed out. If you use only 0.3 ml I believe your needle placement needs to be more precise or you will get a lot of false negative using low volume. I find that nearly 1/3 of the time, especially at L5, when I check a declined view my needle tip is actually half way up the SAP and not close enough to the MB for a low volume injection. I use the "more precise" technique to satisfy my OCD. However, the additional radiation exposure and time involved probably make that a foolish choice.
Wats s “decline” view?I see two schools of thought. You can place your needle in the vicinity of the medial branch as seen on a 15-20 degree oblique view without your superior endplate parallel to the x-ray beam, inject 1 ml of contrast followed by 1ml LA. You will have more false positives and more failed RFN. In exchange you will have a lot less radiation exposure, move quicker and have more RFN billed out. On the opposite end you can make certain endplate is square, check a declined view and make certain your needle tip is in the SAP/TP sulcus and then get away with 0.3 ml of contrast and LA. In exchange you get a lot more radiation exposure, and less RFN billed out. If you use only 0.3 ml I believe your needle placement needs to be more precise or you will get a lot of false negative using low volume. I find that nearly 1/3 of the time, especially at L5, when I check a declined view my needle tip is actually half way up the SAP and not close enough to the MB for a low volume injection. I use the "more precise" technique to satisfy my OCD. However, the additional radiation exposure and time involved probably make that a foolish choice.
I don't understand the role of contrast in an MBB.
If you touch os at the jxn of the TP/SAP I would assume you're there and the procedure is done.
What more is there to confirm or do?
Why run live fluoro and soak up talent extra radiation?
Lol Gluck getting that approved#str8ablate
#neverMBB
It's shown in the SIS technique. Tilt the II toward the feet. If you are on target, in the TP/SAP sulcus, the needle will point obliquely into the sulcus and you will see the tip right in the groove. If you are not in the sulcus you will see the needle tip climb up on the SAP. Yes, extra time and radiation. I use contrast too. I find that there is often vascular uptake and sometimes the contrast flow in a direction away from the groove. Again, extra time and radiation.Wats s “decline” view?
Can you post a link or something to this?It's shown in the SIS technique. Tilt the II toward the feet. If you are on target, in the TP/SAP sulcus, the needle will point obliquely into the sulcus and you will see the tip right in the groove. If you are not in the sulcus you will see the needle tip climb up on the SAP. Yes, extra time and radiation. I use contrast too. I find that there is often vascular uptake and sometimes the contrast flow in a direction away from the groove. Again, extra time and radiation.
Can you post a link or something to this?
I think it's that SIS technique where you line up endplate for given facet level, then oblique ipsilateral 25 degrees and caudal tilt ~45 degrees. then you go co-axial with needle into the junction of the SAP/TP. when you turn AP, the needle is perfectly oblique by Barton's point. On lateral it is perfectly angulated , overlaying the TP but remains posterior to foramen. It's a sweet method but technically you should be adjusting the endplate at every level so then it becomes kind of time intensive in the private practice setting to be quite honest.
Also similarly for cervical medial branch, you caudal tilt until you see the Z joint lines. then you ipsilateral oblique 30 degrees. then you move needle co-axial to the beam and you'll get perfect placement onto the articular pillars in oblique and parasagittal fashion... but again you're supposed to technically adjust for each level with the caudal tilt.
Someone please correct me if i'm wrong. These were techniques i would have liked to really master in fellowship but never got around to it...
Can you post a link or something to this?
Since you bring up the SIS cervical MB RFN technique which recommends a 30 degree ipsilateral oblique approach, I'm curious how many on this forum actually oblique that much?I think it's that SIS technique where you line up endplate for given facet level, then oblique ipsilateral 25 degrees and caudal tilt ~45 degrees. then you go co-axial with needle into the junction of the SAP/TP. when you turn AP, the needle is perfectly oblique by Barton's point. On lateral it is perfectly angulated , overlaying the TP but remains posterior to foramen. It's a sweet method but technically you should be adjusting the endplate at every level so then it becomes kind of time intensive in the private practice setting to be quite honest.
Also similarly for cervical medial branch, you caudal tilt until you see the Z joint lines. then you ipsilateral oblique 30 degrees. then you move needle co-axial to the beam and you'll get perfect placement onto the articular pillars in oblique and parasagittal fashion... but again you're supposed to technically adjust for each level with the caudal tilt.
Someone please correct me if i'm wrong. These were techniques i would have liked to really master in fellowship but never got around to it...
