I don't pay anything for NYT, but I think you need to create a free account. Anyway, here it is.
Can somebody copy and past the text? It is behind a paywall. Thnx
In Military Care, a Pattern of Errors but Not Scrutiny
Photo
A VETERAN’S AGONY Jon Guill of Elgin, Okla., who served in Iraq, preparing formula for his son, Justen, who was born with severe brain damage. Credit Brandon Thibodeaux for The New York Times
FORT SILL, Okla. — Jessica Zeppa, five months pregnant, the wife of a soldier, showed up four times at Reynolds Army Community Hospital here in pain, weak, barely able to swallow and fighting a fever. The last time, she declared that she was not leaving until she could get warm.
Without reviewing her file, nurses sent her home anyway, with an appointment to see an oral surgeon to extract her wisdom teeth.
Mrs. Zeppa returned the next day, in an ambulance. She was airlifted to a civilian hospital, where despite relentless efforts to save her and her baby, she suffered a miscarriage and died on Oct. 22, 2010, of complications from severe sepsis, a bodywide infection. Medical experts hired by her family said later that because she was young and otherwise healthy, she most likely would have survived had the medical staff at Reynolds properly diagnosed and treated her.
Continue reading the main story
Share Your Experiences With Military Health Care
If you have had a first-hand experience with the nation’s military’s health care system, as a patient, family member or worker, please tell us your story by filling out the form below. To leave a comment about this article, click on the comment bubble at top right.
“She was 21 years old,” her mother, Shelley Amonett, said. “They let this happen. This is what I want to know: Why did they let it slip? Why?”
The hospital doesn’t know, either.
Since 2001, the Defense Department has required military hospitals to conduct safety investigations when patients unexpectedly die or suffer severe injury. The object is to expose and fix systemic errors, often in the most routine procedures, that can have disastrous consequences for the quality of care. Yet there is no evidence of such an inquiry into Mrs. Zeppa’s death.
The Zeppa case is emblematic of persistent lapses in protecting patients that emerged from an examination by The New York Times of the nation’s military hospitals, the hub of a sprawling medical network — entirely separate from the scandal-plagued veterans system — that cares for the 1.6 million active-duty service members and their families.
Internal documents obtained by The Times depict a system in which scrutiny is sporadic and avoidable errors are chronic.
As in the Zeppa case, records indicate that the mandated safety investigations often go undone: From 2011 to 2013, medical workers reported 239 unexpected deaths, but only 100 inquiries were forwarded to the Pentagon’s patient-safety center, where analysts recommend how to improve care. Cases involving permanent harm often remained unexamined as well.
At the same time, by several measures considered crucial barometers of patient safety, the military system has consistently had higher than expected rates of harm and complications in two central parts of its business — maternity care and surgery.
More than 50,000 babies are born at military hospitals each year, and they are twice as likely to be injured during delivery as newborns nationwide, the most recent statistics show. And their mothers were more likely to hemorrhage after childbirth than mothers at civilian hospitals, according to a 2012 analysis conducted for the Pentagon.
In surgery, half of the system’s 16 largest hospitals had higher than expected rates of complications over a recent 12-month period, the American College of Surgeons found last year. Four of the busiest hospitals have performed poorly on that metric year after year.
Continue reading the main story
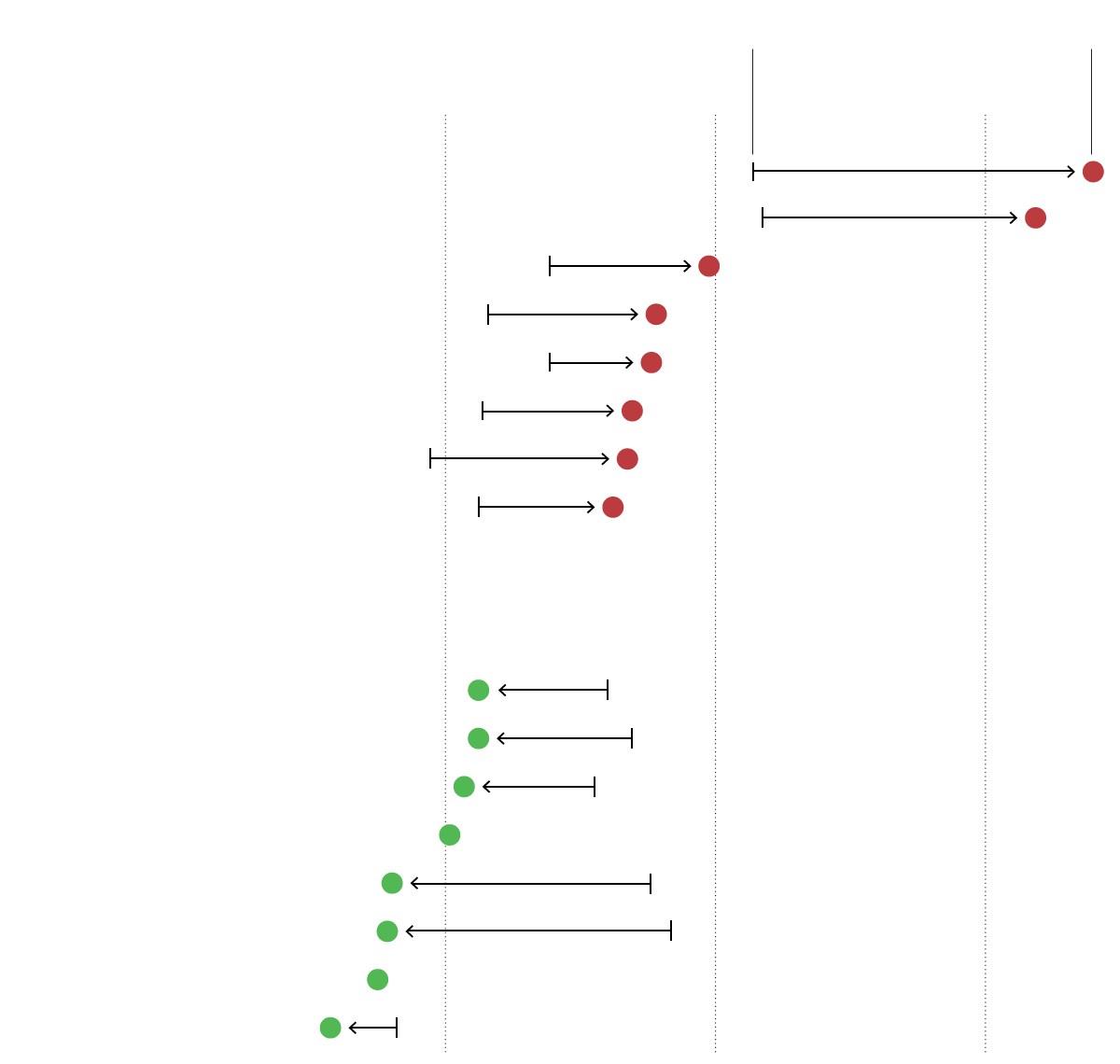
Surgical Complications
Half of the military’s largest hospitals performed worse than established benchmarks in categories such as infections or improperly done procedures, according to a review from the American College of Surgeons. The college compared each hospital with an expected rate of complications based on the procedures it performed and what kinds of patients it served from July 2012 to June 2013.
Expected rate
Actual rate
Hospitals with high rates of surgical complications:
Madigan Army Medical Center
San Antonio Army Medical Center
Naval Medical Center San Diego
Mike O’Callaghan Federal Med. Center
Portsmouth Naval Hospital
Womack Army Medical Center
Fort Belvoir Community Hospital
Evans Army Community Hospital
Hospitals with normal or low rates of surgical complications:
David Grant Medical Center
Tripler Army Medical Center
Wm. Beaumont Army Med. Center
Carl R. Darnall Army Med. Center
Eisenhower Army Medical Center
Walter Reed Nat. Milit. Center
Blanchfield Army Cmty. Hospital
Naval Hospital Jacksonville
Sources: Department of Defense, American College of Surgeons.
Little known beyond the confines of the military community, the Pentagon’s medical system has recently been pushed into the spotlight. In late May, Defense Secretary Chuck Hagel ordered a review of all military hospitals, saying he wanted to determine if they had the same problems that have shaken the veterans system.
Mr. Hagel said the review would study not just access to treatment, the focus of investigations at the veterans hospitals, but also quality of care and patient safety — issues that The Times has been looking at, and asking the Pentagon about, for months.
Defense Department health officials say their hospitals deliver treatment that is as good as or better than civilian care, while giving military doctors and nurses the experience they may one day need on the battlefield. In interviews, they described their patient-safety system as evolving but robust, even if regulations are not always followed to the letter.
“We strive to be a perfect system, but we are not a perfect system, and we know it,” said Dr. Jonathan Woodson, assistant secretary of defense for health affairs. He added, “We must learn from our mistakes and take corrective actions to prevent them from reoccurring.”
The Times’s examination, based on Pentagon studies, court records, analyses of thousands of pages of data, and interviews with current and former military health officials and workers, indicates that the military lags behind many civilian hospital systems in protecting patients from harm. The reasons, military doctors and nurses said, are rooted in a compartmentalized system of leadership, a culture of interservice secrecy and an overall failure to make patient safety a top priority.
The investigations of unforeseen deaths or permanent harm, called root-cause analyses, are widely regarded as a centerpiece of efforts to make care safer. Asked about the military’s missing inquiries, Dr. James P. Bagian, director of the University of Michigan’s Center for Healthcare Engineering and Patient Safety, said, “If in fact unexpected deaths were reported and ignored, there would appear to be no good answer for that except that someone is sleeping at the switch.”
Avoidable errors can and do occur at the best of hospitals. But the military’s reports show a steady stream of the sort of mistakes that patient-safety programs are designed to prevent.
The most common errors are strikingly prosaic — the unread file, the unheeded distress call, the doctor on one floor not talking to the doctor on another. But there are also these, sprinkled through the Pentagon’s 2011 and 2012 patient-safety reports:
A viable fetus died after a surgeon operated on the wrong part of the mother’s body.
A 41-year-old woman’s healthy thyroid gland was removed because someone else’s biopsy result had been recorded on her chart.
A 54-year-old retired officer suffered acute kidney failure and permanent hearing loss after an incorrect dose of chemotherapy.
Such treatment failures are known as “never events,” because they are potentially so grave — and so preventable. They do not happen frequently. But a persistent rate of such mistakes can indicate broader patterns of slipshod care.
Malpractice suits can also be a rough indicator of risk. From 2006 to 2010, the government paid an annual average of more than $100 million in military malpractice claims from surgical, maternity and neonatal care, records show. It would be paying far more if not for one salient reality of military health care: Active-duty service members are required to use military hospitals and clinics, but unlike the other patients, they may not sue. If they could, the Congressional Budget Office estimated in 2010, the military’s paid claims would triple.
Experience in civilian hospitals, and in the veterans system, has shown that stricter procedures and more sophisticated surveillance can limit errors, sometimes markedly. Among some in the military network, concerns about patient safety are longstanding, if rarely acknowledged in public. But calls for change have consistently foundered in the convoluted bureaucracy.
The military health system is split into three major branches, with the Army, Navy and Air Force each controlling its own hospitals and clinics. The Pentagon’s Defense Health Agency also runs the Walter Reed National Military Medical Center and Fort Belvoir Community Hospital, both outside Washington. Any systemwide change involves a carefully calibrated consensus of three equally ranked surgeons general, as well as the Defense Health Agency. Dr. Woodson, who oversees the system, cannot order the surgeons general to act. He can only recommend.
Progress can be glacial: In 2007, for example, the military started rewriting regulations for handling events that harmed or endangered patients. It finished only last October. Several former Pentagon officials said embarrassing statistics were often filtered out, glossed over or buried amid larger data sets before they reached senior health leaders. Two measures used in major civilian hospitals to monitor quality of care — rates of death and readmission, adjusted for seriousness of illness — are simply not tracked.
“The patient-safety system is broken,” Dr. Mary Lopez, a former staff officer for health policy and services under the Army surgeon general, said in an interview.
“It has no teeth,” she added. “Reports are submitted, but patient-safety offices have no authority. People rarely talk to each other. It’s ‘I have my territory, and nobody is going to encroach on my territory.’ ”
In an internal report in 2011, the Pentagon’s patient-safety analysts offered this succinct conclusion about military health care: “Harm rate — unknown.”
Lethal Medical Errors
Katie Guill checked into the hospital at Fort Leonard Wood, Mo., on Christmas morning 2008, expecting to give birth to a healthy baby boy. She left with an infant so severely brain-damaged that at age 5, he cannot crawl, speak or swallow. He must be fed through a pump.
In the three hours before a doctor finally delivered their son, Justen, by cesarean section, the Guills said in a lawsuit, a monitor sounded 32 alerts that the baby’s heart rate had slowed. The suit also said the nurse had warned the doctor on duty four times that the baby was in distress before he arrived at Mrs. Guill’s bedside. The family’s lawyer, Laurie Higginbotham, said she believed the outcome might have been different had the nurse alerted the doctor’s superiors.
Photo
A SON’S INCAPACITY Jon and Katie Guill with Justen, 5. They said fetal distress went unaddressed at Fort Leonard Wood, Mo. Credit Brandon Thibodeaux for The New York Times
The government settled the case for $10 million, but Pentagon records give no indication that a safety investigation was conducted. Nor is there a record of any action taken against the doctors and nurses involved. A spokeswoman said the Defense Department was legally prohibited from discussing how any specific case had been handled.
“We don’t know what went wrong because no one has ever told us,” said Justen’s father, Jon Guill, a former Army mechanic who served 18 months in Iraq.
The Pentagon had promised to look harder at such mistakes.
In 1999, the Institute of Medicine estimated that medical errors killed between 44,000 and 98,000 patients at hospitals nationwide every year. Those numbers — which most experts now consider an undercount — stunned the medical community and kick-started an aggressive effort to protect patients from accidental harm.
Simply penalizing doctors and nurses for malpractice had failed, the institute concluded, because most mistakes arose from weak procedures, not reckless individuals. It called for new strategies, including mandating that medical workers report mistakes and hospitals investigate and correct the lapses that allowed them to occur.
The Pentagon embraced the report, requiring that military treatment facilities produce a written root-cause analysis within 45 days in all cases of unexpected serious injury or death. “Such events are called ‘sentinel’ because they signal the need for immediate investigation and response,” the regulations state. Military hospitals must also report sentinel events to the Joint Commission, an independent accreditation group. Specialists at the Pentagon’s patient-safety center, created in 2001, were told to review the analyses and recommend changes.
Certainly it is difficult to assess such a divided and diverse medical system, with 56 hospitals, domestic and overseas, ranging from the flagship, Walter Reed, to a hospital in the middle of the Mojave Desert with an average of three inpatients a day. They serve not only young, typically healthy active-duty families but also the longest-serving military retirees and their families. Even so, experts say safety reviews can reveal trouble spots as well as patterns of error across an entire system.
But annual patient-safety reports and other internal documents obtained by The Times show that, for years, the center’s analysts have often found themselves staring into darkness.
Photo
CHALLENGES AHEAD Justen cannot crawl, speak or swallow. Credit Brandon Thibodeaux for The New York Times
As early as 2003, a Pentagon audit noted that medical workers had reported 80 cases of severe harm or death in the preceding 12 months, but that only 32 root-cause analyses had been forwarded to the center. Five years later, another audit concluded, “Unfortunately, R.C.A.s are used relatively infrequently.”
The most recent safety reports paint a similar — and more detailed — picture.
In 2011, 50 unexpected deaths were identified but only 25 analyses submitted.
The next year, the center was informed of 110 deaths but received only 44 root-cause analyses.
And in 2013, the report documented 79 deaths and 31 root-cause analyses.
The safety audits also make clear that of the root-cause analyses that are done, the cases of clearest-cut blame — the “never events” — make up the largest group. Even so, the reports show, those mistakes have not subsided.
In 2010, the safety center had sounded a hopeful note. For the first time in nine years, it said, “all surgeries and procedures were performed on the right person.” But the next year, the center said surgeons were still performing the wrong procedure or operating on the wrong patient or part of the body at an “alarming” rate. It called for intensive hospital audits to lower it.
Last year, medical workers reported virtually the same number of errors. They also reported more cases in which medical devices were inadvertently left inside patients than they had four years earlier.
In a written response to questions from The Times, the Pentagon acknowledged that it had taken a decade before the reporting system was “operational and collecting data in a uniform manner.” Not until last October, for instance, were the Army, Navy and Air Force required to identify the facilities where patients were severely harmed or died.
Senior defense health officials say the missing investigations are not a true measure of attention paid to serious harm. “There are many mechanisms for reviewing significant adverse events,” the Pentagon said in a statement.
In an interview, Dr. Woodson said a different kind of inquiry that hospitals conduct — a risk-management investigation — might have gotten to the bottom of what went wrong. Those investigations focus on whether individual doctors or nurses provided substandard care for which the government could be liable.
“I feel confident that we capture and investigate the overwhelming majority of these adverse events,” Dr. Woodson said. “The key is having a robust system and that you pick all of them up and make the changes that are appropriate.”
But military regulations specifically require both types of inquiries, and for good reason, patient-safety experts say: Otherwise, even catastrophic errors — mistakes for which no one is specifically to blame, but that instead result from systemic lapses — can be easily swept under the rug.
Busy but Troubled Hospital
Womack Army Medical Center in Fort Bragg, N.C., is one of the system’s largest, busiest hospitals. Lately it has also been one of its more troubled.
For three years, it has had a higher-than-average rate of surgical complications, and in March it suspended all elective surgery for two days after inspectors found problems with surgical infection controls. Then last month, the Army ousted the hospital’s leadership after the unexpected deaths of two patients in their 20s: a mother of three who had undergone a low-risk surgical procedure and a soldier who had been sent home from the emergency room.
That same day, Defense Secretary Hagel ordered the systemwide review.
At Womack and elsewhere, some doctors and nurses complain that no one listens to their safety warnings. One staff member interviewed by The Times recalled filing roughly 50 reports of safety problems since 2007, each time providing contact information. Only once, the worker said, did a supervisor respond, and then only to express irritation at the fusillade of filings.
“It is an exercise in futility,” said the staff member, speaking on condition of anonymity for fear of job repercussions. “We can jump up and down and shake our fists, but nothing changes.”
Dr. Lopez, the former Army staff officer, said some hospital officials had told her that they felt pressure from superiors to focus on budget cutting and efficiency, while patient safety got a cursory nod.
Across the system, Pentagon officials cite some signs of progress. In 2008, for instance, the composite rate of 11 types of harm — like pressure ulcers and postoperative hemorrhages — was more than twice that of civilian hospitals with a similar patient mix. Last year, it was better than the civilian average, although the Pentagon’s own analysts warned results might be skewed by reporting problems.
Even so, the most recent patient-safety report complained of a general lack of headway in building a safer system. While the number of reports of harm has varied over the last decade, and “there are certainly pockets of excellence,” it noted, “The leading trends remain consistent.” What was needed was “enterprisewide change.”
The operating room has been one focus of concern.
The study by the American College of Surgeons found that in addition to Womack, three other major hospitals — Madigan Army Medical Center in Tacoma, Wash.; San Antonio Army Medical Center in Texas; and Portsmouth Naval Hospital in Virginia — have had high rates of surgical complications for two or three years in a row. Five of the eight cited last year had also been flagged repeatedly for high rates of infection related to surgery.
Dr. Brian Lein, the Army’s deputy surgeon general, said hospitals that fell below the benchmark “have dug deep into the data to find the actual issues and are addressing those issues.” The Navy echoed that response.
With so many young military families, the system’s maternity wards are among its busiest. Pentagon officials say maternity care is top notch, and on some leading measures of safe childbirth, the military hospitals indeed compare well with their civilian counterparts.
For example, their rate of infant mortality was equal to or lower than that of civilian hospitals in the most recent data analyzed by the National Perinatal Information Center, a private group with a Pentagon contract. In routine vaginal births, the rate of injury to the mother has consistently been below the national average.
On other measures, though, the military system lags.
In 40 percent of the military hospitals, mothers were significantly more likely to suffer hemorrhages after birth than at the civilian hospitals tracked by the perinatal center. The hemorrhages can lead to hysterectomies or even death. About 2,500 cases were recorded in military hospitals in 2012, roughly 760 more than if the military had met the civilian benchmark.
If doctors used instruments such as forceps to assist the delivery, mothers in military hospitals were about 15 percent more likely to be injured than mothers nationally, the most recent data shows.
One of the broadest measures of safe childbirth is the rate of injuries to babies, ranging from cerebral hemorrhages to small cuts on babies’ scalps. From 2009 to 2011, according to a Times analysis, the rate at military hospitals was twice the national average.
In 2011, nearly five in every 1,000 babies born at military hospitals suffered some kind of birth trauma. Had the military met the national average, 107 newborns would have been injured instead of 239.
Dr. Woodson said the military is looking “closely at areas where we are falling short” on maternity care and measuring its hospitals against civilian ones in order to improve.
Ordeal Giving Birth
When Stephanie King felt labor pains on Easter in 2004, she drove to Reynolds Army Community Hospital. She was 34, a kindergarten teacher and mother of two. Her husband, an Army artillery officer, was serving six months in Iraq, so her 12-year-old son accompanied her to the hospital.
Her contractions were coming every three to five minutes, court records show, but a resident on the maternity ward refused to admit her, saying her cervix was not sufficiently dilated. The attending physician agreed.
Photo
DEAF AFTER A HOSPITAL ORDEAL Dawson King contracted an infection when he was born in 2004 after the Fort Sill hospital kept his mother, despite contractions, from being admitted in time to be given antibiotics. Credit Drew Angerer for The New York Times
Mrs. King spent the next two hours in the hospital’s first-floor lobby, waiting room, cafeteria and bathroom. She wanted to seek care at the civilian hospital 15 minutes away, but her military insurance would not cover it. In the midst of her ordeal, her husband called from Baghdad to say he was being airlifted to Germany after an emergency appendectomy.
Finally, fearful that she would deliver on the bathroom floor, she took the elevator back to maternity. A nurse greeted her with what seemed to be a joke: " ‘Oh, Mrs. King, you are back,’ ” she recalled the nurse saying. " ‘You don’t look as good as you did when you first came in.’ ”
Any amusement vanished, however, when staff members realized not only that Mrs. King was about to give birth — but that her file showed she carried a common but symptomless strain of group B streptococcus bacteria. Women in labor must be given antibiotics at least an hour before delivering to avoid transmitting the infection to their newborns, hospital workers later testified.
Dawson King was born just 42 minutes after his mother was admitted. Doctors soon determined that he had contracted an infection, and warned Mrs. King that the only effective medication could cause deafness. Four months later, when Dawson did not turn his head when his parents walked into the room, it became clear that he was profoundly deaf.
Continue reading the main story
Only three years later, after Mrs. King filed a malpractice claim, was the case discussed at Reynolds, court records indicate. The attending physician said a risk-management meeting was held to ensure that the standard of care was met. No report was written, and the doctors and the nurse emerged with spotless licenses.
That result that would appear to point to a lapse in hospital procedures. But both the resident and the nurse testified that they had never attended a meeting at Reynolds to discuss what had gone wrong.
“That’s the disturbing part,” Mrs. King said, while Dawson draped himself over the arm of his father’s chair, looking at photos of himself as a 1-year-old, his head swathed in bandages from surgery for cochlear implants. “Doesn’t the hospital want to know what happened?”
Photo
'A SUCCESS STORY' Dawson, who had surgery for cochlear implants when he was 1, is now an engaging, soccer-playing 10-year-old. Still, his mother said, “It was devastating how easily it could have been prevented.” Credit Drew Angerer for The New York Times
Mrs. King believes that she knows: Her file documented her history of strep B infection and the fact that her second child had been born after a 90-minute labor. And the resident testified that he could not recall if he had read her record before declining to admit her. “It boils down to they did not even read my records,” Mrs. King said.
The government settled the Kings’ case in 2009 for $300,000. Mrs. King describes her son, now an engaging, soccer-playing 10-year-old, as “a success story.” Still, she said, “it was devastating how easily it could have been prevented.”
The Kings’ malpractice payout was relatively modest. An examination of court records and Pentagon data from Reynolds and seven other hospitals turned up dozens of settlements, ranging from $30,000 to $10 million, but no record of a root-cause analysis.