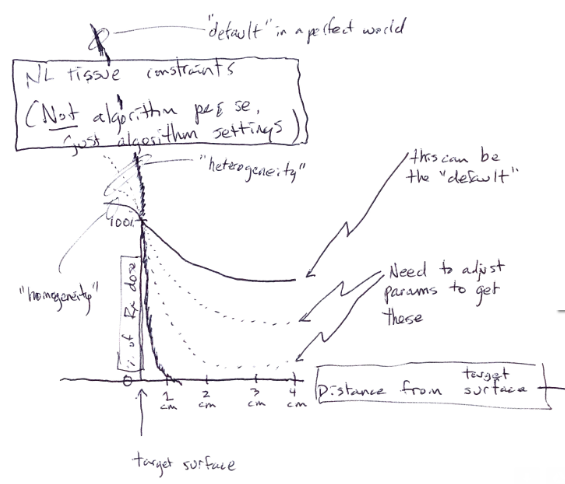
There are differences there and they mainly have to do with normal tissue contraints.
We don't push the fractionated dose higher in the brain. We give 3 x 11 Gy (or 3 x 9 Gy @80% isodose à la Minniti) or 6 x 6 Gy (@95% isodose) for brain mets, but won't push much higher than that. These doses are considered suboptimal for the treatment of primary tumors in the lung or metastases in the lung or liver from any tumor. Earlier SBRT series point out at a high risk of local failure (>30%) when giving doses like that, people were careful in the early SBRT days and we have the data.
But would you be comfortable with giving 3 x 25 Gy (or let's say 3 x 15 Gy @ 60% isodose) to a brain metastasis (à la Timmemann for NSCLC-primaries)?
Actually the Japanese have done something similar for GBM.
Hypofractionated high-dose IMRT with concurrent and adjuvant TMZ altered the dominant failure pattern from localized to disseminated and prolonged the survival of patients with GBM. Necrosis in the SVZ was associated with better patient survival, but the benefit of radiation to this area remains...

www.ncbi.nlm.nih.gov
8 x 8.5 Gy to the GTV. Now that's a dose you would consider "curative" if you would give it to a T1-NSCLC in the lung, right? It's practice a lot, for example for primaries close/in the "no-fly-zone"
Roughly 50% radionecrosis when the same dose was given to GBMs...
It's the same with the bone. 1 x 20 Gy or 2 x 10 Gy are acceptable SBRT schedules.
We don't push higher than that, because of toxicity constraints regarding spinal cord and nerves (and possibly bone fractures).
I've treated with 1 x 34 Gy only once. Metastatic NSCLC patient sent for palliative RT of painful bone mets. His 2cm primary was not far from where we treated the bone mets and we just gave it 1 x 34 Gy, so that it wouldn't cause any problems in the future. 1 x 34 Gy is only feasible with small tumors which are not adjacent to the chest wall (unless you are comfortable with high single-doses to the ribs, which I am not) or centrally located. All of these lesions can easily be treated with 3 x 25 Gy, which is probably also "more" in terms of BED (using the linear-quadratic-model with these high single doses is not well validated, but my gut feeling is that 3 x 25 Gy > 1 x 34 Gy).
What we are experiencing in NSCLC-SBRT fractionation is the opposite of brain-mets-SRS fractionation.
We used to fractionated more in NSCLC and modern trials have tried to fractionated less for some primaries (mainly peripheral) while optimize fractionation for others, where high toxicity was noted with large fraction doses (mainly the no-fly-zone, after toxicities were seen with 3-fraction-schedules). Brain-SRS was the domain of single-shot (mainly GK) SRS and is now being switched to more fractionated treatments, especially for larger lesions and post-operative cavities.